
I'm a huge fan of keeping others safe from harmful people and harmful situations.
ANNOUNCEMENT
December, 2025 Coming February - March 2026. New helpful material and various resources. From positive-inspirational to the many ways to fight back against evil and corruption, along with protest, boycott, event information, etc. (until no longer applicable 🥺).
Additionally I will be blogging and vlogging about my authentic life, the MANY struggles, battles and the accomplishments despite it all. *Sharing things no one knows about me.
Keep scrolling to learn more about me.
🤍💙
Thank you for your patience during the platform's transition.
STAY TUNED ~ Stay safe ~ Stay Aware ~ Be Kind ~ Be Authentic ~ Stay HUMBLE 🤍🕊️💙
Platform last updated, 1/15/2026 Fixsensadnessforhs.com (Fixsen-Sadness-For-Humanity's Suffering & Humanity's Solidarity).
NOTE: I do NOT give the Hidradenitis Suppurativa (HS) "non-profit" organization (name can be provided by request), or ANY of their affiliates permission to use my materials, ideas, experiences, or collected study information for ANY of their needs and/or used on their website, or on their social media platform (s). Disclaimers of the plagiarism are noted on some of my material. All other material will be listed in future blogging.
About
FREQUENTLY ASKED QUESTIONS
What is Hidradenitis Suppurativa (HS)?
Hidradenitis Suppurativa is a non-contagious inflammatory
illness that causes painful abscesses (boil-like), nodules underneath the skin, skin tunneling, and scarring (often extensive). Millions of people around the world are afflicted. It can have a significant impact on individuals, affecting them in various ways, including physically, mentally, socially, emotionally, spiritually, and financially.
Like many illnesses, the exact cause (s) remain unknown. It has been established for more than ten years that HS is a chronic inflammatory illness, with involvement of follicular occlusion, microbiome, and biofilm.
HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger.
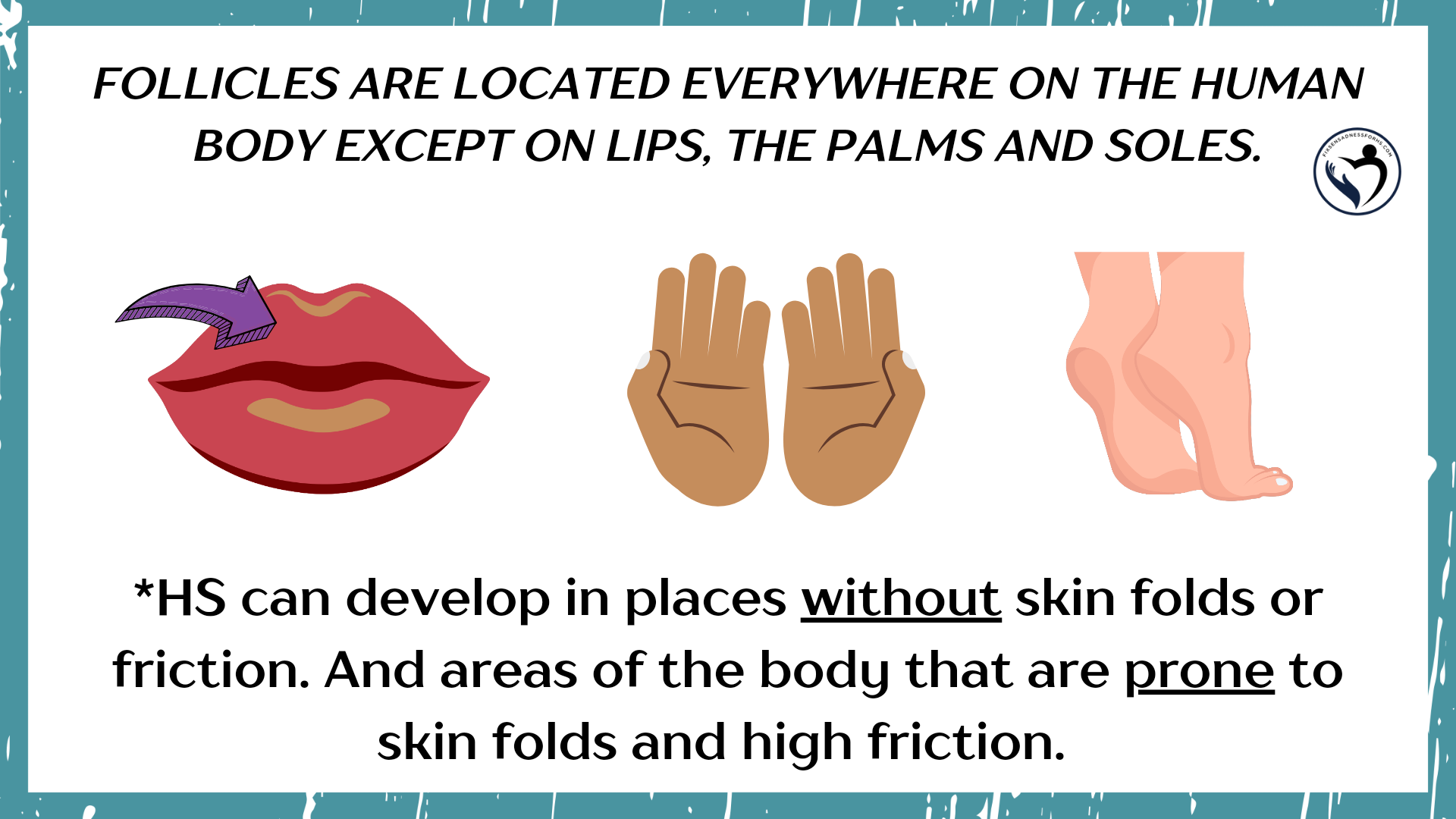
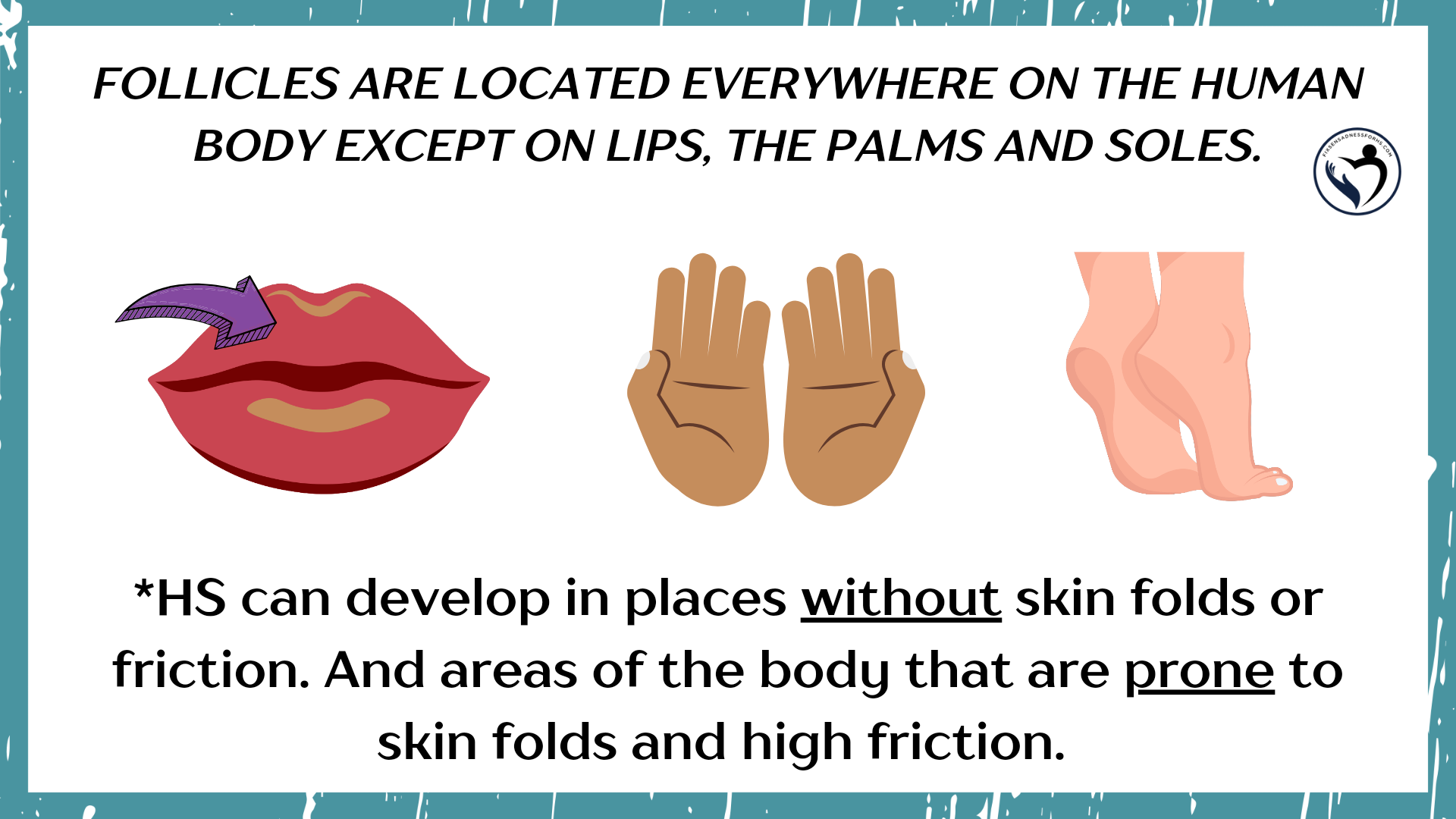
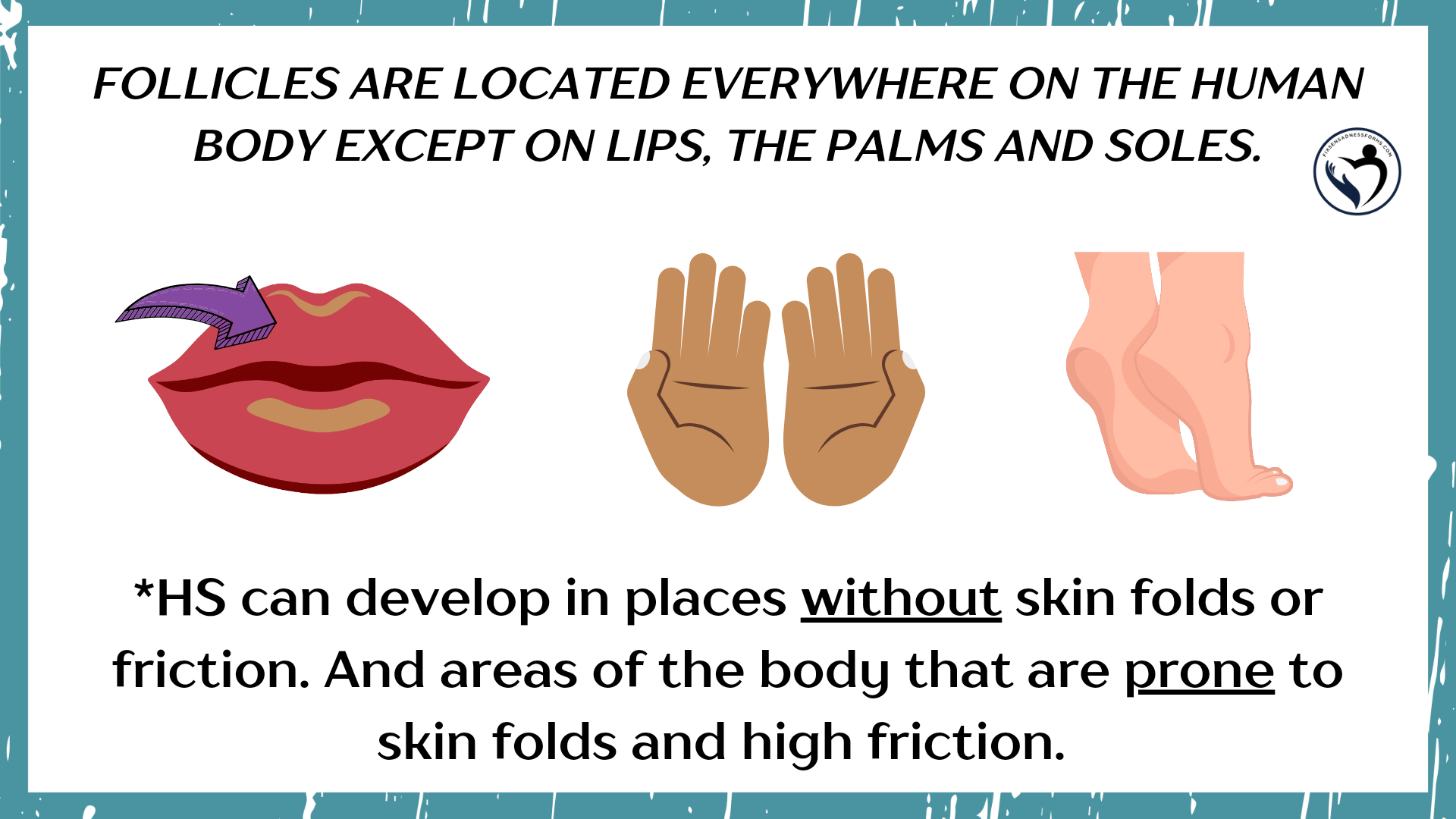
Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. With a few exceptions, abscesses (“boil-like”) and nodules can manifest in any area of the body, excluding ON the lips, palms of hands, and soles of feet.
 It is possible for HS to occur in the ears and in the nose. HS cannot be developed internally within the body (on organs, intestines, etc.).
It is possible for HS to occur in the ears and in the nose. HS cannot be developed internally within the body (on organs, intestines, etc.).
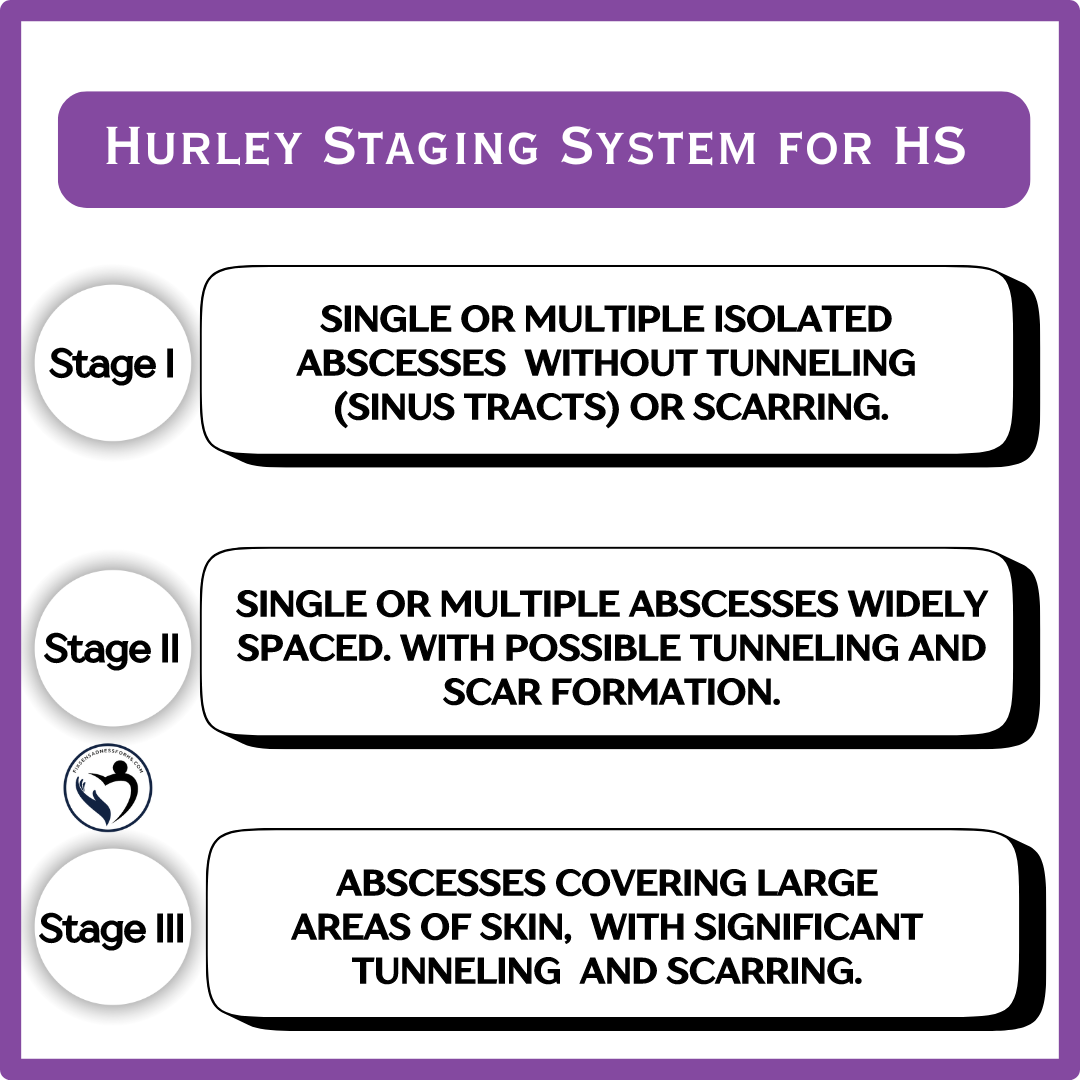
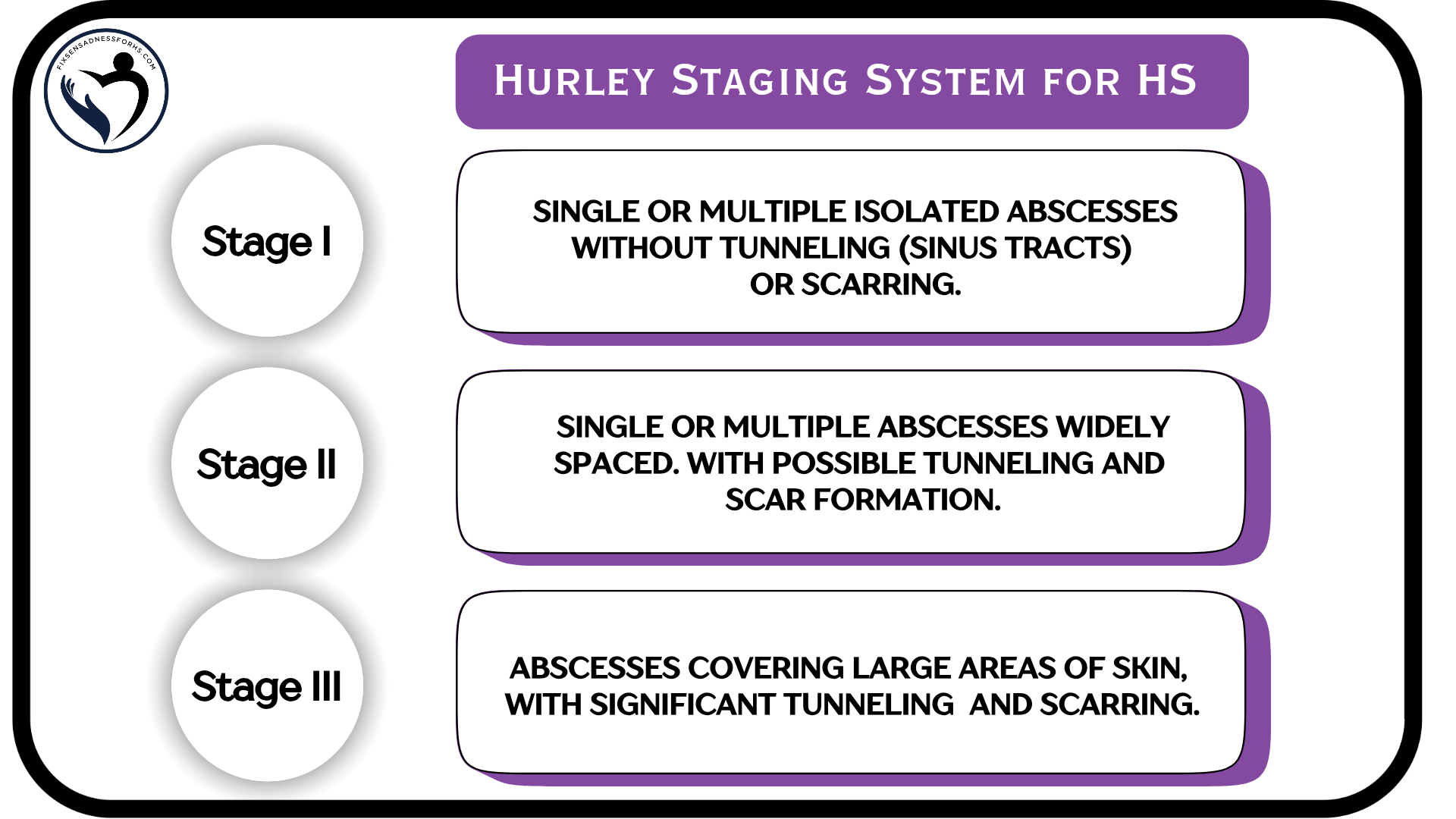
HS has three stages (III) using the Hurley staging system.
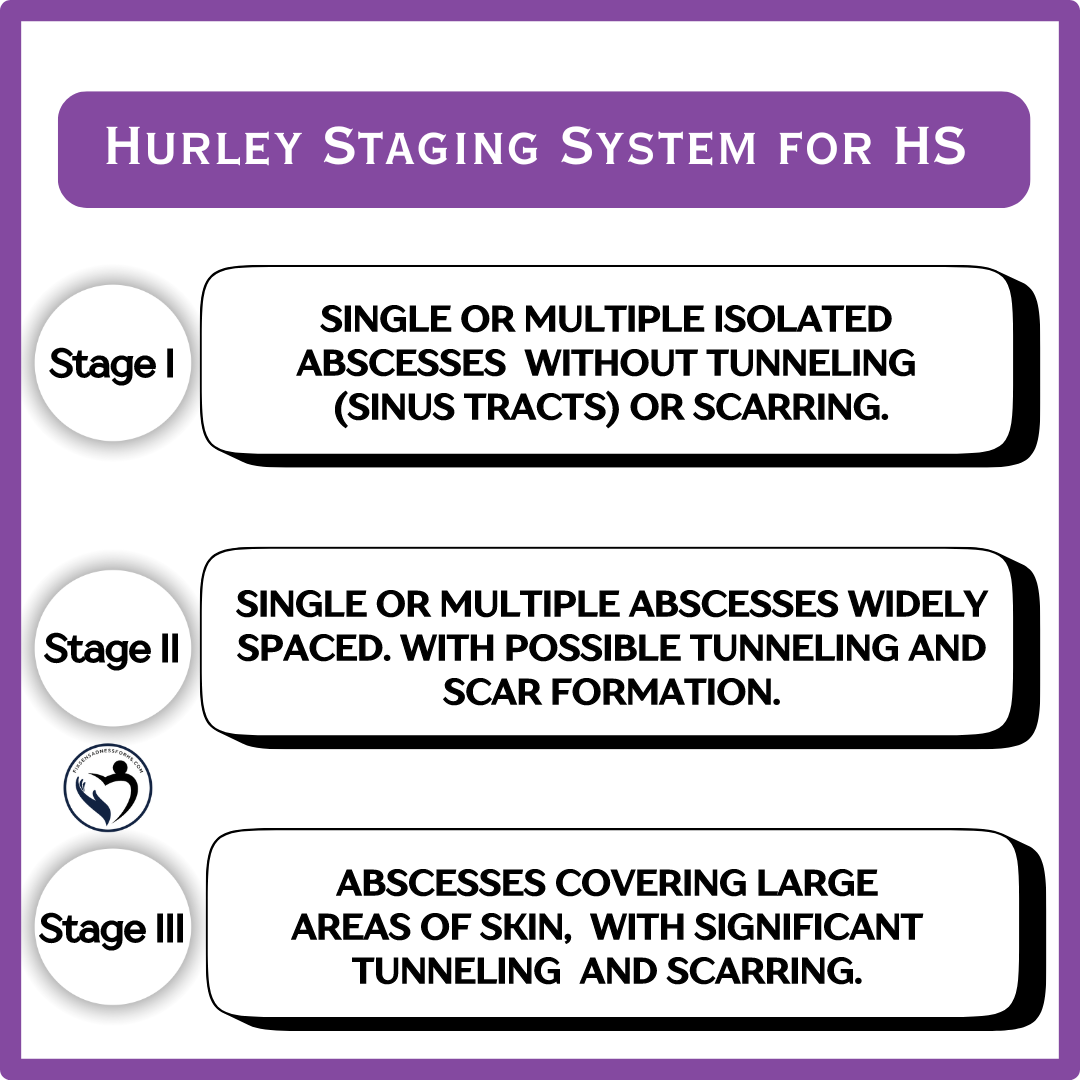 You can have various Hurley stages (I, II, III) on different areas of the body.
You can have various Hurley stages (I, II, III) on different areas of the body.
Some Facts:
Research is always ongoing. The complexity of the immune system is truly extraordinary. Our bodies and HS exhibit a great deal of complexity. Experts may find out there is a place for both auto-inflammatory and autoimmune as they do share common features, but for now, chronic inflammatory illness, with a follicular occlusion involvement, and microbiome, and biofilm components is what long-standing research & pathology supports.
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources: PMC7450471, PMID:32884675, doi:10.1001/jamadermatol.2017.0904, doi.org/10.1016/j.clindermatol.2023.08.021, PMC8537933, PMID:34696185, PMC8324042,
doi.org/10.1186/s43162-021-00040-5
FAQ posted on 08-25-2024
illness that causes painful abscesses (boil-like), nodules underneath the skin, skin tunneling, and scarring (often extensive). Millions of people around the world are afflicted. It can have a significant impact on individuals, affecting them in various ways, including physically, mentally, socially, emotionally, spiritually, and financially.
Like many illnesses, the exact cause (s) remain unknown. It has been established for more than ten years that HS is a chronic inflammatory illness, with involvement of follicular occlusion, microbiome, and biofilm.
HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger.
Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. With a few exceptions, abscesses (“boil-like”) and nodules can manifest in any area of the body, excluding ON the lips, palms of hands, and soles of feet.
 It is possible for HS to occur in the ears and in the nose. HS cannot be developed internally within the body (on organs, intestines, etc.).
It is possible for HS to occur in the ears and in the nose. HS cannot be developed internally within the body (on organs, intestines, etc.). HS has three stages (III) using the Hurley staging system.
 You can have various Hurley stages (I, II, III) on different areas of the body.
You can have various Hurley stages (I, II, III) on different areas of the body.Some Facts:
- The classification of HS as a gland disease was debunked years ago.
- Antibiotics are primarily prescribed for their anti-inflammatory properties unless there is an infection present. If an infection occurs, it is considered a secondary complication.
- Having other illnesses or comorbidities does not alter the classification of HS.
- Hidradenitis Suppurativa affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination
- It is not an infectious illness (not contagious)
- HS meets the criteria for a chronic inflammatory illness that has been established.
- But its not that simple
- Research has specifically provided evidence with HS for auto-inflammatory, the innate immune system, and its role in the immune system overreacting.
- HS has never been categorized as an autoimmune condition There is no substantial, long-standing research or pathology that fully meets the criteria. Autoimmune is the adaptive immune system, where healthy tissues are mistakenly identified as foreign and are attacked.
Research is always ongoing. The complexity of the immune system is truly extraordinary. Our bodies and HS exhibit a great deal of complexity. Experts may find out there is a place for both auto-inflammatory and autoimmune as they do share common features, but for now, chronic inflammatory illness, with a follicular occlusion involvement, and microbiome, and biofilm components is what long-standing research & pathology supports.
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources: PMC7450471, PMID:32884675, doi:10.1001/jamadermatol.2017.0904, doi.org/10.1016/j.clindermatol.2023.08.021, PMC8537933, PMID:34696185, PMC8324042,
doi.org/10.1186/s43162-021-00040-5
FAQ posted on 08-25-2024
How many stages of HS are there?
Three stages (III) using the Hurley Staging System.
The Hurley staging system is the first staging tool developed for hidradenitis suppurativa by Dr. Harry James Hurley Jr., an American dermatologist, in 1989. And it continues to be a highly utilized tool for assessing HS severity. Across the world.
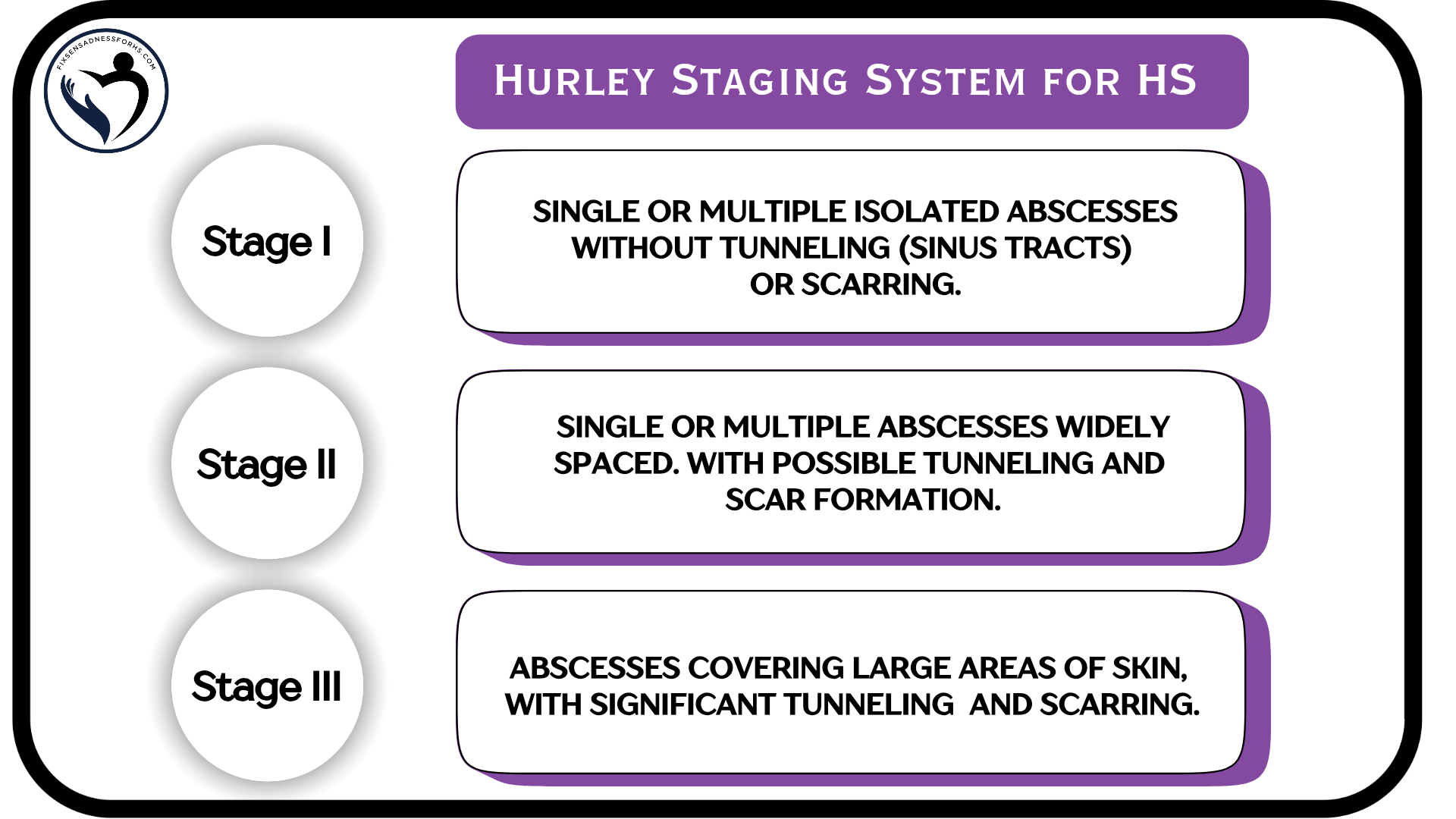 This tool is used to classify patients with HS into three disease severity groups.
This tool is used to classify patients with HS into three disease severity groups.
*You can have different stages in different areas of your body and you can also be between stages.
Please see various stages in reference photos below (may be considered graphic).
The Hurley staging system is the first staging tool developed for hidradenitis suppurativa by Dr. Harry James Hurley Jr., an American dermatologist, in 1989. And it continues to be a highly utilized tool for assessing HS severity. Across the world.
 This tool is used to classify patients with HS into three disease severity groups.
This tool is used to classify patients with HS into three disease severity groups.*You can have different stages in different areas of your body and you can also be between stages.
Please see various stages in reference photos below (may be considered graphic).
Reference pics HERE
Reference pics HERE
Reference pics HERE
It’s important to note that hidradenitis may appear differently on skin of color. Depending on the person’s skin tone, it can be flesh-colored, pink, purple, brown, gray, or blackish.
Please see reference photos below:
Reference photo 1
Reference Photo 2
Reference Photo 3
Reference Photo 4
Tidbit - There are approximately 11 other HS scoring systems for various purposes, such as treatment evaluation, surgery assessments, insurance, clinical trials, and disability.
I will explore this topic further in my article (which will be linked to this section) in the near future.
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources: doi:10.5114/reum.2018.80709, DOI: 10.2340/00015555-2513, doi.org/10.33235/wpr.30.1.40-49, PMCID: PMC10149852
Volume 41, Issue 5, The Authors (of doi:10.1111/bjd.17588). British Journal of Dermatology published by John Wiley & Sons Ltd on behalf of British Association of Dermatologists.
FAQ posted on 08-26-2024
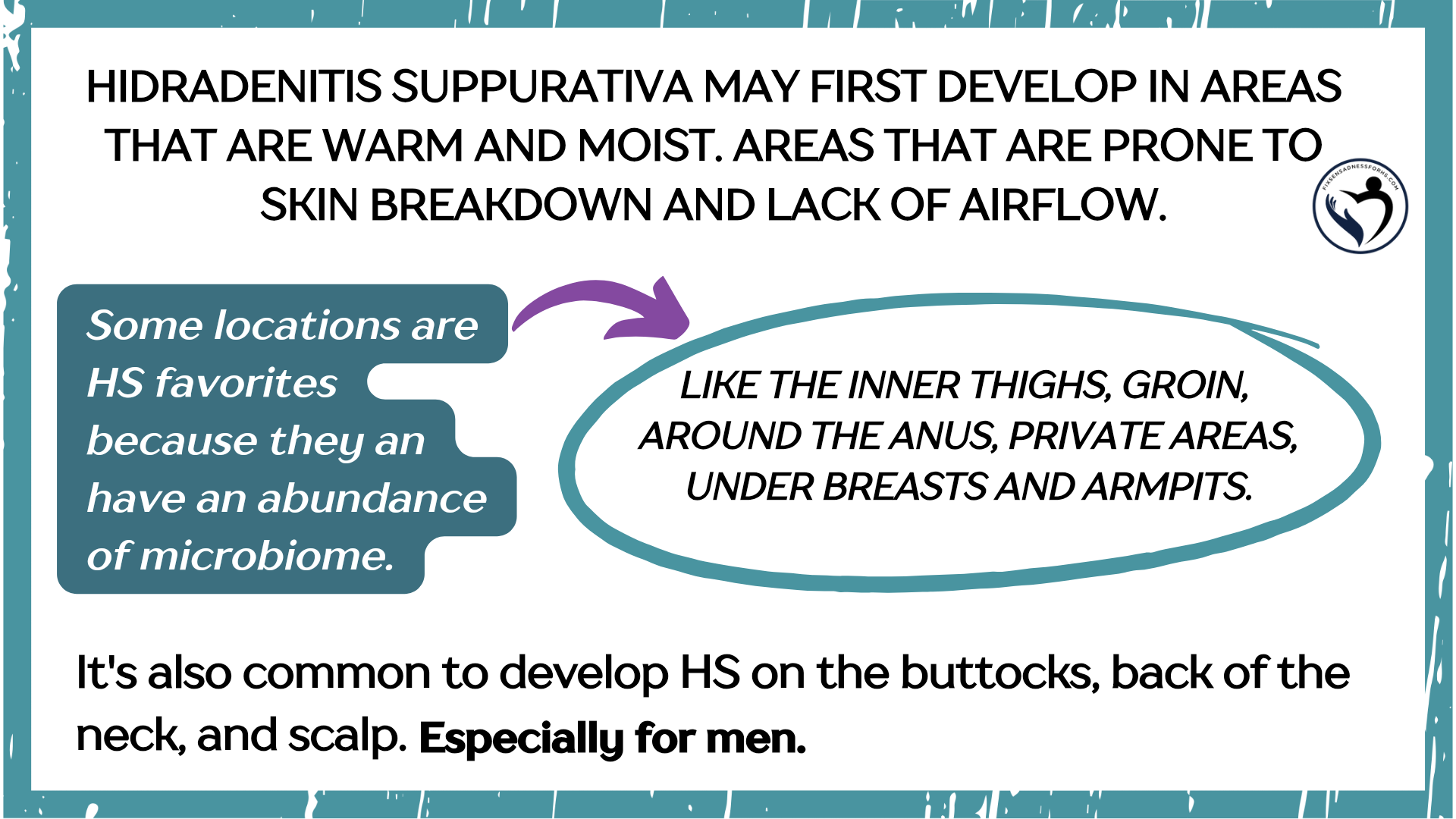
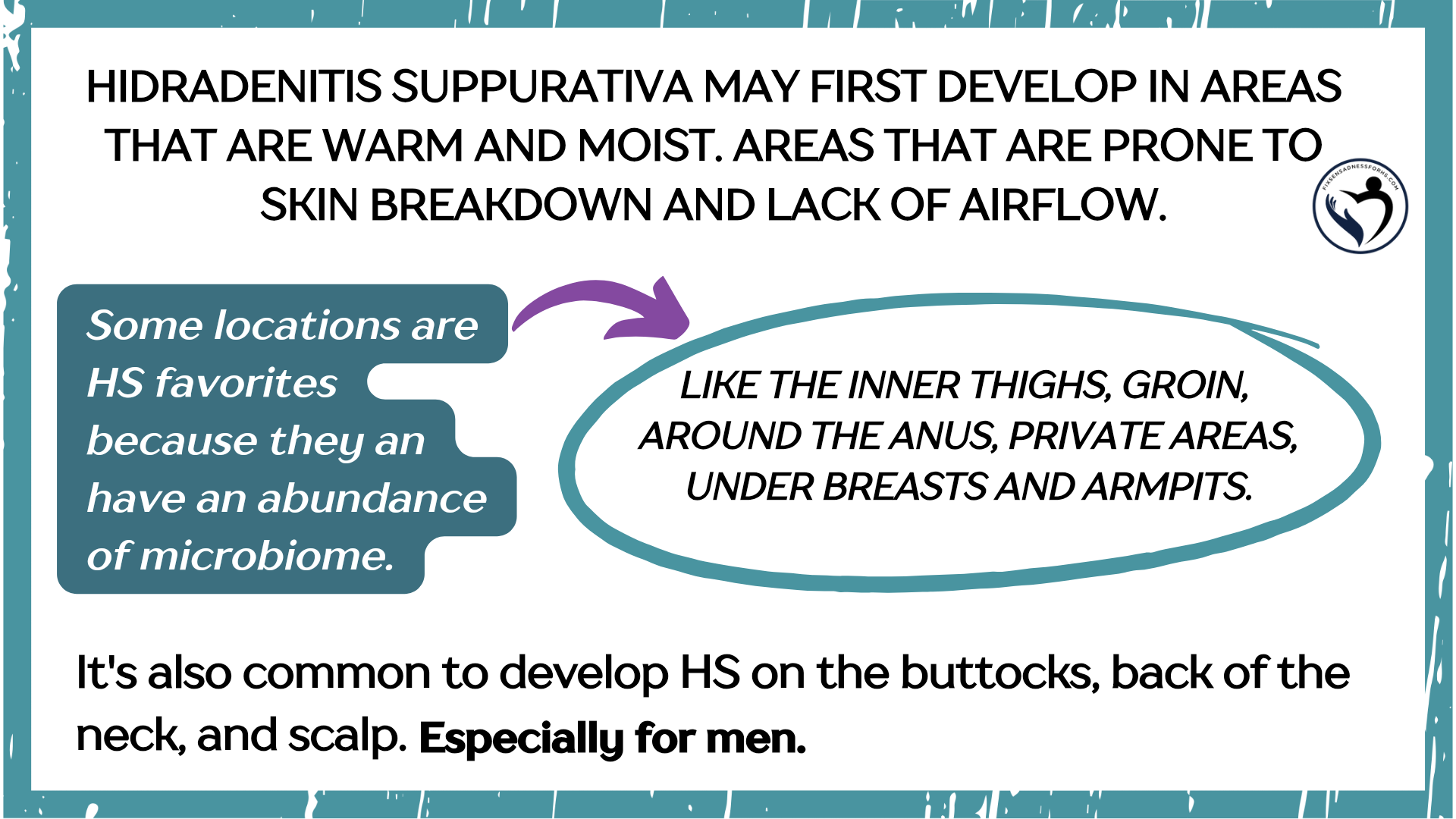
Where can HS occur on the body?
Hidradenitis suppurativa can develop anywhere follicles are found. Follicles are located everywhere on the human body except ON lips, palms, and soles.
 It is possible for HS to occur in the ears and in the nose. HS cannot be developed internally within the body (on organs, intestines, etc.).
It is possible for HS to occur in the ears and in the nose. HS cannot be developed internally within the body (on organs, intestines, etc.). HS can develop in places without skin folds or friction. And areas of the body that are prone to skin folds and high friction.
In summary HS can show up in various places, from head to toe and everywhere in between.
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
PMCID:PMC7450471
PMID: 32884675 doi:10.1001/jamadermatol.2017.09 doi.org/10.1016/j.clindermatol.2023.08.021 PMCID:PMC9570026
PMID: 36232581 PMCID:PMC3535073
PMCID:PMC8362278
PMID: 34409370
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
PMCID:PMC7450471
PMID: 32884675 doi:10.1001/jamadermatol.2017.09 doi.org/10.1016/j.clindermatol.2023.08.021 PMCID:PMC9570026
PMID: 36232581 PMCID:PMC3535073
PMCID:PMC8362278
PMID: 34409370
What is tunneling and sinus tracts?
Tunneling - this may also be referred to as skin tunnels or sinus tracts.
This process typically happens with Hurley stages 2 & 3. It is when reoccurring HS abscesses and bumps turn into tunnels beneath the skin. With chronic inflammation.
Tunneling or sinus tract formation starts under the skin. They are connected to the abscesses and / or several abscesses within the surrounding area. Channels that go from the skin to deeper tissue.
View images here:
I will explore this topic further in my article (which will be linked to this section) in the near future.
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
doi.org/10.1016/j.jaci.2020.12.651
Image Credit: JACI Journal of Allergy and Clinical Immunology, American Academy of Allergy, Asthma & Immunology.
FAQ posted on 08-27-2024
doi.org/10.1016/j.jaci.2020.12.651
Image Credit: JACI Journal of Allergy and Clinical Immunology, American Academy of Allergy, Asthma & Immunology.
FAQ posted on 08-27-2024
Are blackheads normal with HS?
Yes! However, these "blackhead-like" are far from ordinary. They are technically called double-ended pseudocomedones, (DEP) or sometimes referred to as double-ended comedones.
DEP’s are signs of HS that are often overlooked. Nevertheless, they are deemed a standard clinical sign of HS. And play an important role in helping clinicians diagnose Hidradenitis Suppurativa.
DEP’s are identified as coupled hollows surrounded by whitish cicatricial tissue during dermoscopic examination ((the examination of the skin using skin surface microscopy). Keratin was found to be accumulating. Under histopathological examination (study of diseased cells and tissues using a microscope), they were identified as large hollows with dilated superficial openings.
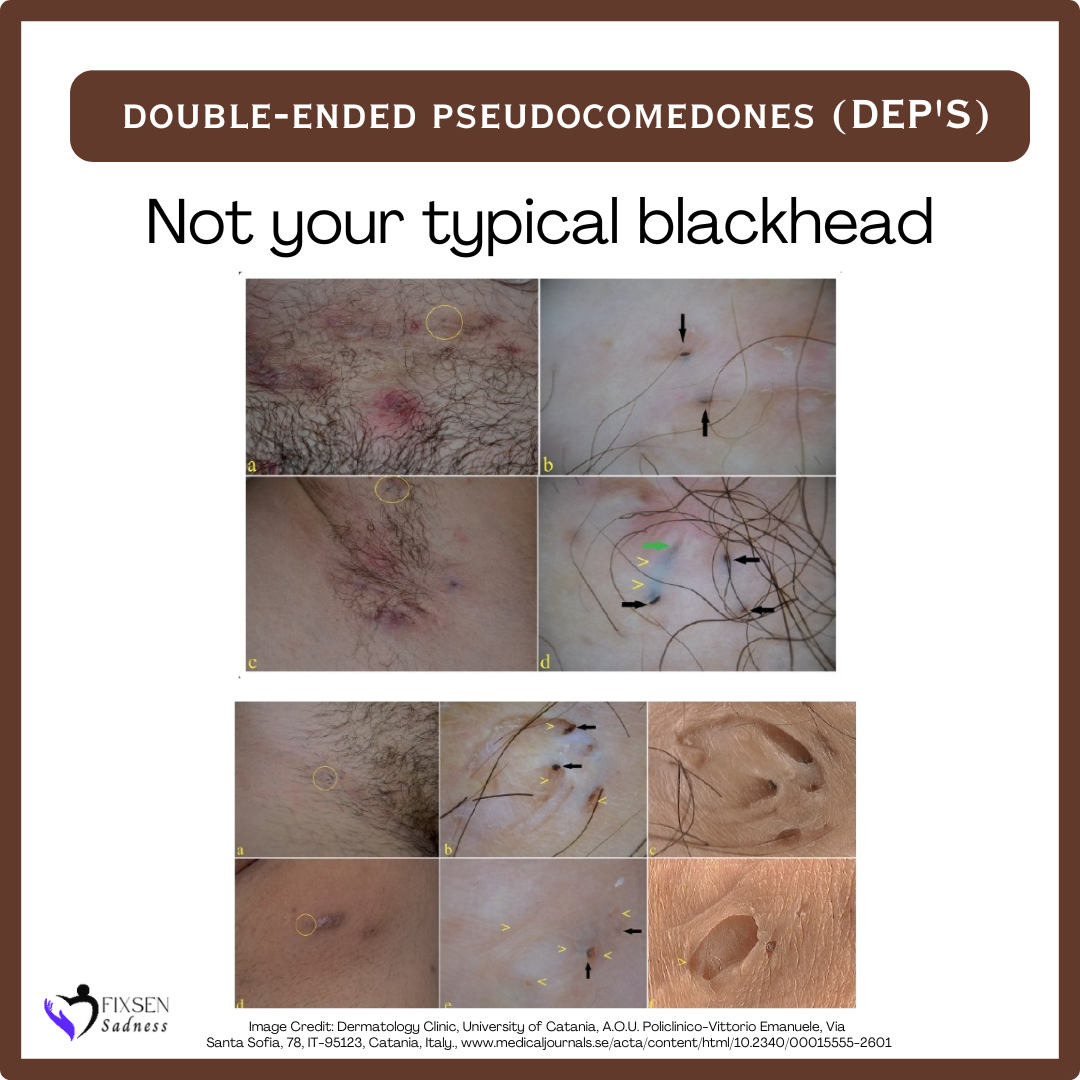
Most DEP's are a result of the healing of previous inflammatory lesions.
It’s also common for individuals with HS to experience whiteheads and pimple-like bumps.
To prevent further harm and potential HS flares, refrain from picking or squeezing.
I will go into this topic more thoroughly in the future in my article (will be tagged to this section). Including tips on how to better manage.
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
doi.org/10.1016/j.jaad.2017.04.415 doi:10.2340/00015555-2601
Image Credit: Dermatology Clinic, University of Catania, A.O.U. Policlinico-Vittorio Emanuele, Via Santa Sofia, 78, IT-95123, Catania, Italy.
FAQ posted on 08-29-2024
DEP’s are signs of HS that are often overlooked. Nevertheless, they are deemed a standard clinical sign of HS. And play an important role in helping clinicians diagnose Hidradenitis Suppurativa.
DEP’s are identified as coupled hollows surrounded by whitish cicatricial tissue during dermoscopic examination ((the examination of the skin using skin surface microscopy). Keratin was found to be accumulating. Under histopathological examination (study of diseased cells and tissues using a microscope), they were identified as large hollows with dilated superficial openings.
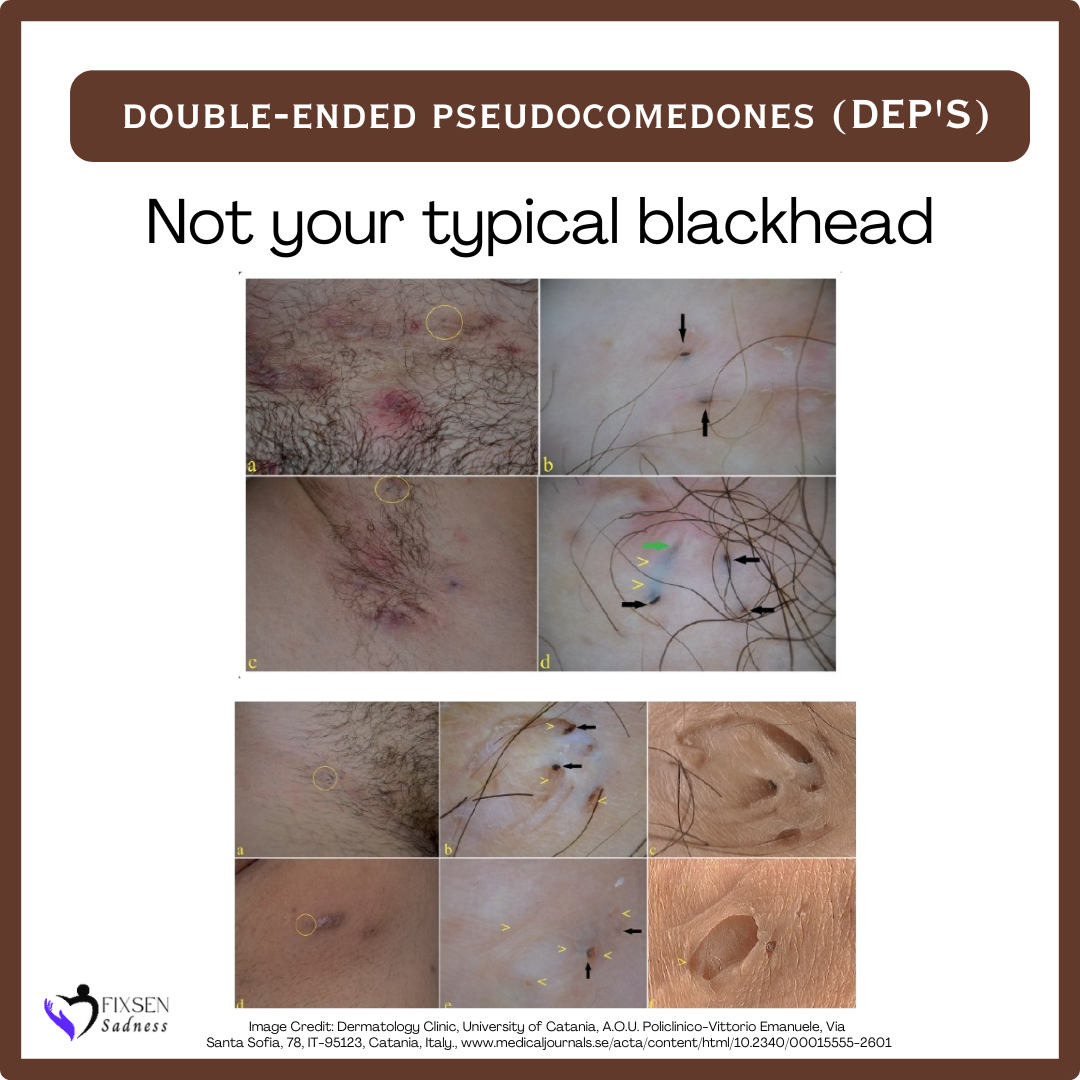
Most DEP's are a result of the healing of previous inflammatory lesions.
It’s also common for individuals with HS to experience whiteheads and pimple-like bumps.
To prevent further harm and potential HS flares, refrain from picking or squeezing.
I will go into this topic more thoroughly in the future in my article (will be tagged to this section). Including tips on how to better manage.
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
doi.org/10.1016/j.jaad.2017.04.415 doi:10.2340/00015555-2601
Image Credit: Dermatology Clinic, University of Catania, A.O.U. Policlinico-Vittorio Emanuele, Via Santa Sofia, 78, IT-95123, Catania, Italy.
FAQ posted on 08-29-2024
Why does HS have an odor?
There are various explanations for this. Below, you’ll find a snapshot.
A few Explanations:
Inflammation, bacteria, breakdown of sweat and skin tissue.
When an abscess contains pus, the pus itself is a combination of dead white blood cells, bacteria (good/bad live/dead), tissue debris, germs, serum, etc.
These environments can produce compounds that result in odor and foul smells.
Note:
The presence of a strong smell does not necessarily mean there is an infection.
It’s common for drainage colors to differ in HS and it doesn’t necessarily indicate an infection.
I will explore this topic further in my article (which will be linked to this section) in the near future.
Special Note: Written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
PMC7450471PMID: 32884675 doi:10.1001/jamadermatol.2017.0904
PMC7450471PMID: 32884675 doi:10.1001/jamadermatol.2017.0904
FAQ posted on 08-29-2024
Is it normal for my blood inflammatory markers to be elevated?
Yes. It’s normal for inflammatory markers to be elevated or high.
HS is an illness that causes inflammation.
Additionally, due to persistent inflammation and trauma (chronic abscesses). And in the case of an infection being present.
As a result, several blood markers could show higher levels.
These may include:
White blood cell (WBC), serum proinflammatory cytokines,
C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), leukocytosis, neutrophils, and monocytes.
The nature of this can be either persistent or intermittent. It varies depending on the severity of the disease.
HS is an illness that causes inflammation.
Additionally, due to persistent inflammation and trauma (chronic abscesses). And in the case of an infection being present.
As a result, several blood markers could show higher levels.
These may include:
White blood cell (WBC), serum proinflammatory cytokines,
C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), leukocytosis, neutrophils, and monocytes.
The nature of this can be either persistent or intermittent. It varies depending on the severity of the disease.
Bear in mind, HS is not responsible for everything. Always speak to your medical team regarding your test results.
I will go into this topic more thoroughly in the future in my article (will be tagged to this section). Including tips on how to better manage.
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
I will go into this topic more thoroughly in the future in my article (will be tagged to this section). Including tips on how to better manage.
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
PMCID: PMC9009384PMID: 35432388
PMCID: PMC9127563PMID: 35620323 doi.org/10.1111/jdv.18175
FAQ posted on 08-29-2024
PMCID: PMC9009384PMID: 35432388
PMCID: PMC9127563PMID: 35620323 doi.org/10.1111/jdv.18175
FAQ posted on 08-29-2024
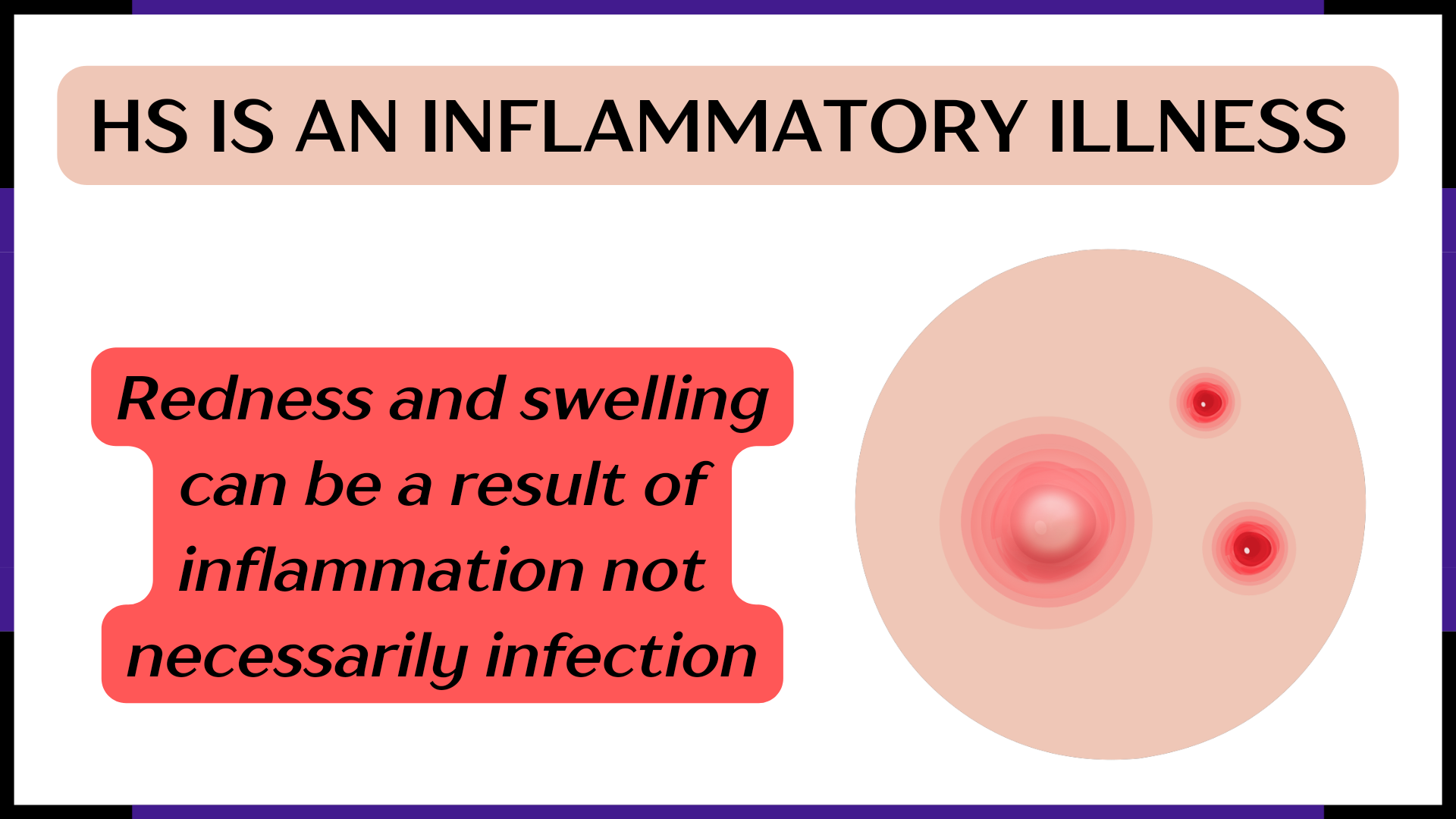
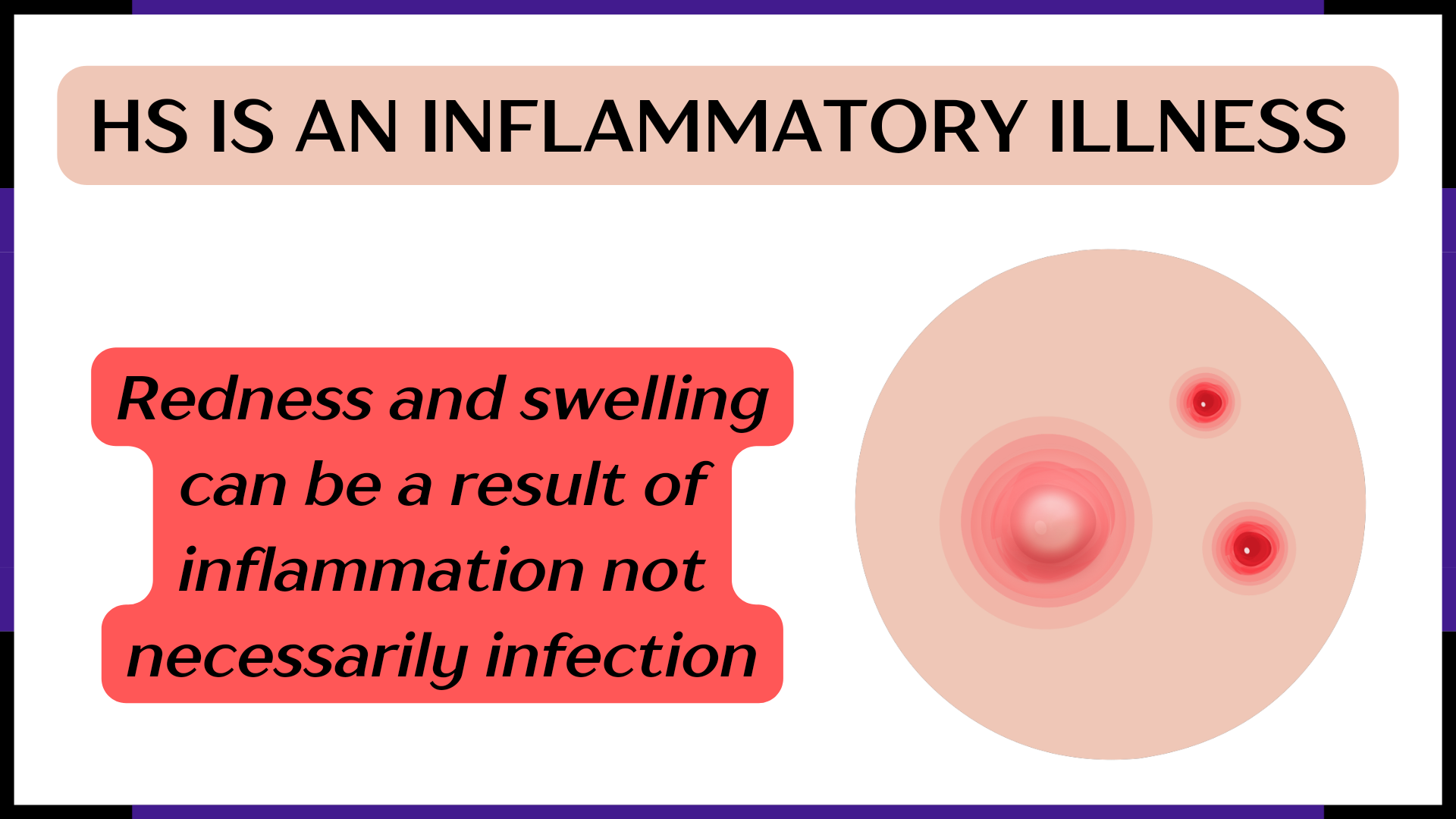
Is my HS always infected, and/or is my body always fighting infection?
Typically, the answer is no (there will always be exceptions).
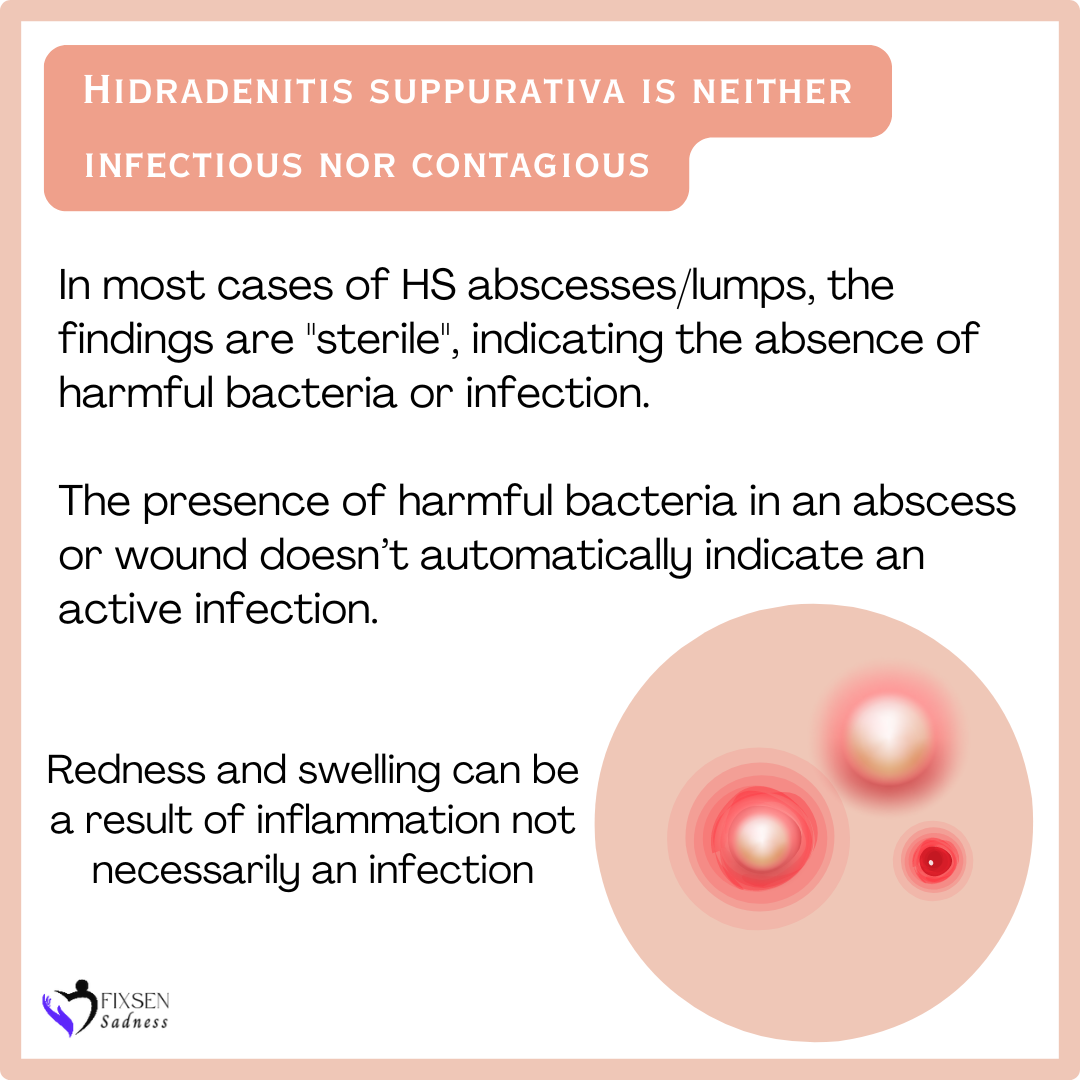
Hidradenitis Suppurativa is neither infectious nor contagious.
Skin bacteria can be identified through standard culture tests, which may reveal both normal and pathogenic bacteria. Culturing an abscess may or may not reveal the presence of harmful bacteria.
Quick Facts:
Hidradenitis Suppurativa is neither infectious nor contagious.
Skin bacteria can be identified through standard culture tests, which may reveal both normal and pathogenic bacteria. Culturing an abscess may or may not reveal the presence of harmful bacteria.
Quick Facts:
- In most cases of HS abscesses/lumps, the findings are sterile, indicating the absence of harmful bacteria or infection.
- In patients with chronic HS, it’s important to take cultures from active deep abscesses with sinus tracts as a precautionary measure.
- When the presence of harmful bacteria in an abscess or wound is found this doesn’t automatically indicate an active infection.
Redness and swelling can be a result of inflammation, not necessarily an infection.
Some factors that can amplify the risk of infection:
•Extracting or manipulating HS troubles areas; abscesses, DEP’s (blackhead-like), etc. through picking or squeezing.
•Self-lancing, the use of needles and squeezing.
•Excessive use of antibacterial products can disrupt the balance of good bacteria.
•Overuse of antibiotics.
Tidbit:
HS is a challenging inflammatory condition. The immune system, hair follicles, follicular occlusion, microbiome disruption, and biofilm components are all interconnected. In addition, there is a connection between HS and gene mutations, familial ties (hereditary), environmental factors, and behavioral influences.
I will go into this topic more thoroughly in the future in my article (will be tagged to this section). Including tips on how to better manage.
Special Note: Researched, compiled, and written by Denise Fixsen, This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.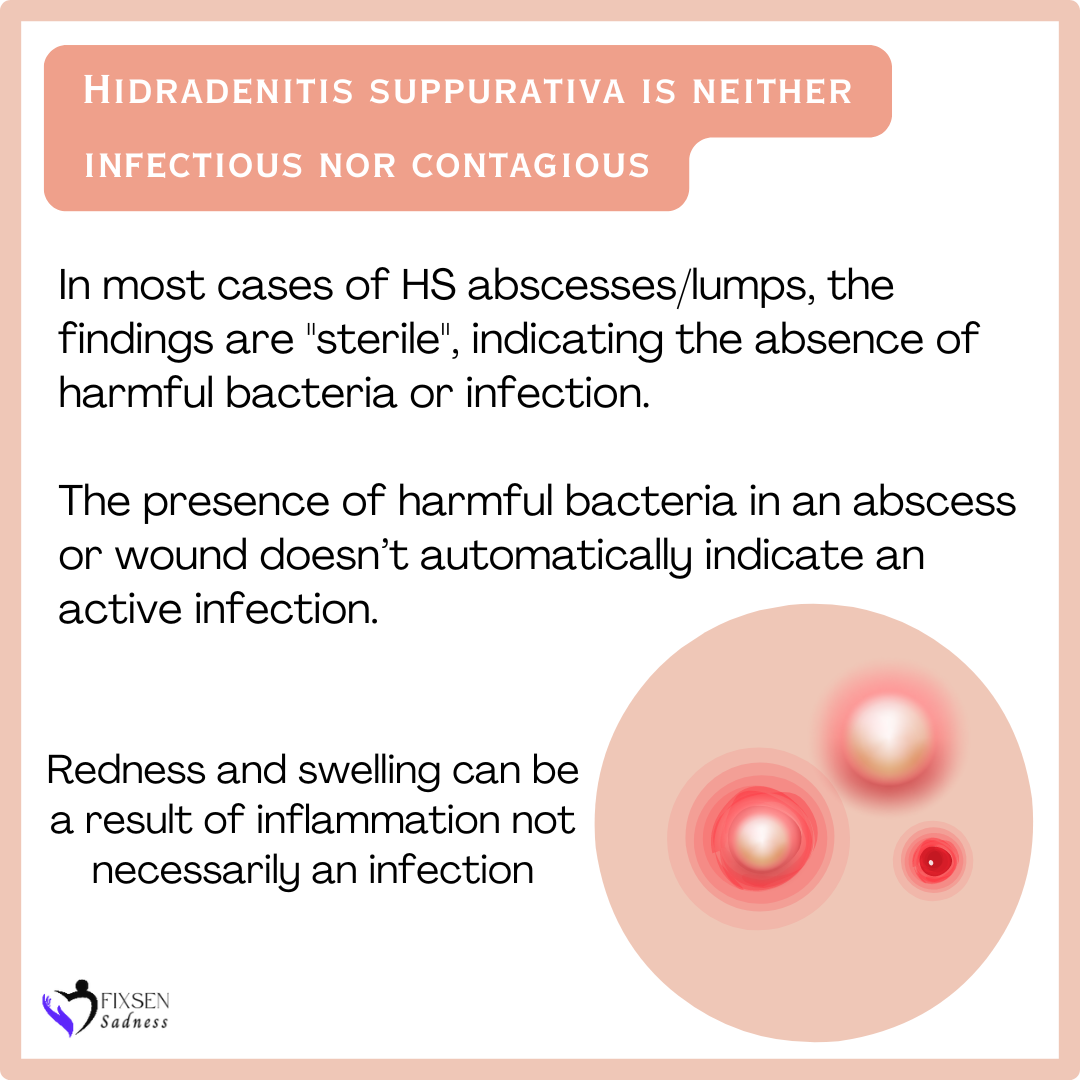
Some factors that can amplify the risk of infection:
•Extracting or manipulating HS troubles areas; abscesses, DEP’s (blackhead-like), etc. through picking or squeezing.
•Self-lancing, the use of needles and squeezing.
•Excessive use of antibacterial products can disrupt the balance of good bacteria.
•Overuse of antibiotics.
Tidbit:
HS is a challenging inflammatory condition. The immune system, hair follicles, follicular occlusion, microbiome disruption, and biofilm components are all interconnected. In addition, there is a connection between HS and gene mutations, familial ties (hereditary), environmental factors, and behavioral influences.
I will go into this topic more thoroughly in the future in my article (will be tagged to this section). Including tips on how to better manage.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
doi.org/10.3389/fmed.2020.00068 Volume 7
PMID: 27382916
Merck Manual Professional Edition
FAQ posted on 09-01-2024
Why are there so many terms for our illness, like sinus tracts, boil-like, pustules, and nodules, etc.?
Let’s dive into the language that is commonly used with HS to help you navigate your journey.
All of these terms below are acceptable and accurate in describing Hidradenitis Suppurativa:- Abscesses, lesions, or boil-like - typically describing HS that is elevated and on top of the skin.
- Nodules, lumps, and bumps - usually beneath the skin.
- DEPs - Blackhead-like - the technical term for them is double-ended pseudocomedones, or sometimes called double-ended comedones.
- Pustules - small, inflamed sores filled with pus.
- Wounds - can occur after an HS abscess drains. These can be acute or chronic.
- Skin tunnels, tunneling, and sinus tracts - channels that go from the skin to deeper tissue.
- Fistulas - an abnormal connection between two epithelial surfaces.
- Scar Tissue, Roped Scaring, Hypertrophic Scarring, Fibrotic, and Keloid Scars - in a pathological process, normal tissue is replaced by connective tissue, leading to the formation of permanent scar tissue.
The terms below do not accurately describe Hidradenitis Suppurativa:
- Boils
- Cysts
- Acne
- Folliculitis
I get why it can be confusing, and it’s totally understandable. If everyone agreed on terminology worldwide, it would be less confusing for everyone, including those in the medical field and researchers.
Together, we have the power and numbers to make a difference in raising awareness about HS. We must keep up with those efforts.
Together, we have the power and numbers to make a difference in raising awareness about HS. We must keep up with those efforts.
I will go into some of these topics more thoroughly in the future in my articles (will be tagged to this section). Including tips on how to better manage.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
PMC7450471PMID: 32884675 doi:10.1001/jamadermatol.2017.0904 doi.10.1016/j.clindermatol.2023.08.021
PMC8537933PMID: 34696185
doi: 10.1007/s00590-019-02432-4
doi: 10.1001/jamadermatol.2017.5978 DOI: 10.3810/pgm.1999.10.1.730 doi.org/10.1159/000529848 doi.org/10.1016/j.ijscr.2022.107196
FAQ posted on 09-01-2024
What is causing me to receive incorrect diagnoses?
Some possible explanations include lack of consistent factual awareness and lack of qualified HS clinicians.
Moreover, Hidradenitis suppurativa is often misdiagnosed in the early stages, as it can be easily mistaken for boils, cysts, acne, ingrown hairs, and folliculitis, particularly by medical professionals unfamiliar with the condition.
Moreover, Hidradenitis suppurativa is often misdiagnosed in the early stages, as it can be easily mistaken for boils, cysts, acne, ingrown hairs, and folliculitis, particularly by medical professionals unfamiliar with the condition.
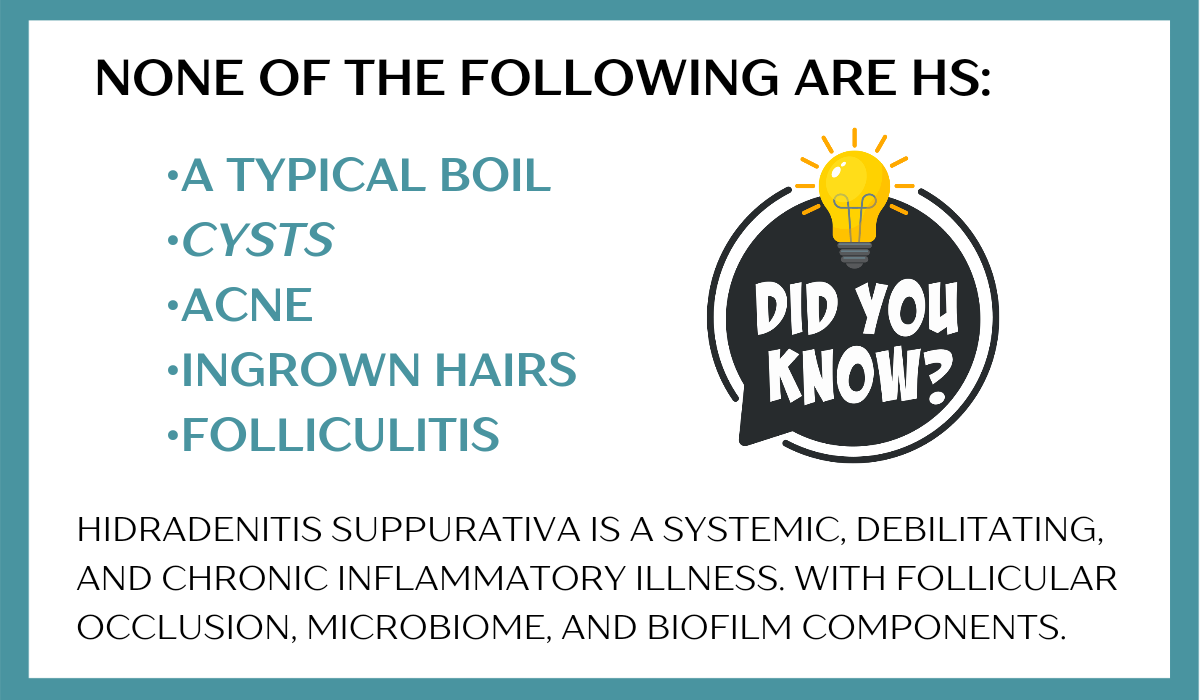
While HS sufferers may be prone to these other conditions, it’s important to understand that HS is distinct from them. By receiving an accurate diagnosis earlier, you can prevent the condition from worsening and enhance your quality of life.
I will go into some of these topics more thoroughly in the future in my articles (will be tagged to this section). Including tips on how to better manage.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
PMC7450471PMID: 32884675 doi:10.1001/jamadermatol.2017.0904 doi.10.1016/j.clindermatol.2023.08.021 PMC8537933PMID: 34696185
doi: 10.1007/s00590-019-02432-4
doi: 10.1001/jamadermatol.2017.5978 DOI: 10.3810/pgm.1999.10.1.730 doi.org/10.1159/000529848 doi.org/10.1016/j.ijscr.2022.107196
FAQ posted on 09-04-2024
How many approved Hidradenitis Suppurativa treatments are there?
Currently, in the USA there are two biologic treatments approved for moderate-to-severe Hidradenitis Suppurativa. There are two medications: Humira (adalimumab) and Cosentyx (Secukinumab).
Approval for Bimzelx (Bimekizumab), a biologic, is anticipated in late 2024 or early 2025, if all goes well.
Several clinical trials are currently underway, and some hold great potential for the future.

Tidbits:
Effective treatment options have been discovered by identifying the sources of inflammatory markers thought to be associated with HS symptoms.
Even though classified as biologics, these medications work differently within the body to treat hidradenitis.
Bimzelx and Cosentyx both target IL-17 (but in distinct ways).
Bimekizumab selectively ‘inhibits both IL-17A and IL-17F
Cosentyx targets and blocks IL-17A.
Humira targets and blocks TNF-alpha
I will go into this topic more thoroughly including countries of drug approval and some history in the future in my article. It will be tagged to this section. Including tips on how to better manage.
The tidbit in this FAQ was inspired by Michael Duguay (HS Warrior).
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
PMCID: PMC10609891
doi: 10.1111/exd.14619
PMCID: PMC8183777
Approval for Bimzelx (Bimekizumab), a biologic, is anticipated in late 2024 or early 2025, if all goes well.
Several clinical trials are currently underway, and some hold great potential for the future.

Tidbits:
Effective treatment options have been discovered by identifying the sources of inflammatory markers thought to be associated with HS symptoms.
Even though classified as biologics, these medications work differently within the body to treat hidradenitis.
Bimzelx and Cosentyx both target IL-17 (but in distinct ways).
Bimekizumab selectively ‘inhibits both IL-17A and IL-17F
Cosentyx targets and blocks IL-17A.
Humira targets and blocks TNF-alpha
I will go into this topic more thoroughly including countries of drug approval and some history in the future in my article. It will be tagged to this section. Including tips on how to better manage.
The tidbit in this FAQ was inspired by Michael Duguay (HS Warrior).
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources:
PMCID: PMC10609891
doi: 10.1111/exd.14619
PMCID: PMC8183777
FAQ posted on 09-10-2024
Is Hidradenitis Suppurativa being researched?
HS has been continuously researched since the 1800’s.
•More than 5,000 research publications have been dedicated to Hidradenitis Suppurativa.
•HS research publications reached a staggering 1,157 between 2023 and 2024. That's a lot of funding and effort.
Research includes genes, genetics, bacteria, comorbidities,
integrative medicine, nutrition, and so MUCH more.
•HS has 47 current clinical trials, including both drug and nondrug options.
•There are currently 2 treatments that have been FDA approved, with another one expected to be approved by the end of 2024 or early 2025. See more on this under the FAQ section HERE, "BIMZELX® (bimekizumab) a possible THIRD FDA approved treatment option on the way"
Research and study on HS have been and will continue to be conducted. Progress is being made rapidly on advancements.
We're not being ignored, and neither is our illness. There is hope!
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources: National Institutes of Health,
Velpeau A. Dictionnaire de Medicine, un Repertoire des Sciences Medicales sons le Rapport, Theorique et Pratique. 2nd ed Paris. 1839. 91.
FAQ posted on 09-13-2024

•More than 5,000 research publications have been dedicated to Hidradenitis Suppurativa.
•HS research publications reached a staggering 1,157 between 2023 and 2024. That's a lot of funding and effort.
Research includes genes, genetics, bacteria, comorbidities,
integrative medicine, nutrition, and so MUCH more.
•HS has 47 current clinical trials, including both drug and nondrug options.
•There are currently 2 treatments that have been FDA approved, with another one expected to be approved by the end of 2024 or early 2025. See more on this under the FAQ section HERE, "BIMZELX® (bimekizumab) a possible THIRD FDA approved treatment option on the way"
Research and study on HS have been and will continue to be conducted. Progress is being made rapidly on advancements.
We're not being ignored, and neither is our illness. There is hope!
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources: National Institutes of Health,
Velpeau A. Dictionnaire de Medicine, un Repertoire des Sciences Medicales sons le Rapport, Theorique et Pratique. 2nd ed Paris. 1839. 91.
FAQ posted on 09-13-2024
