Detailed information on and about Hidradenitis Suppurativa
Hidradenitis Suppurativa is a non-contagious illness characterized by painful abscesses, nodules underneath the skin, skin tunneling, and scarring (often excessive). Millions of people around the world are afflicted. It can have a significant impact on individuals, affecting them in various ways, including physically, mentally, socially, emotionally, spiritually, and financially. The feeling of isolation and being misunderstood can have a deep impact.
HS has been extensively studied since the 1800s and continues to be. Like many illnesses, the exact cause(s) remain unknown. However, it has been established for more than ten years that HS is a chronic inflammatory illness, with involvement of follicular occlusion, microbiome, and biofilm components.
HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger.
Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. With a few exceptions, abscesses (“boil-like”) and nodules can manifest in any area of the body, excluding ON the lips, palms of hands, and soles of feet.
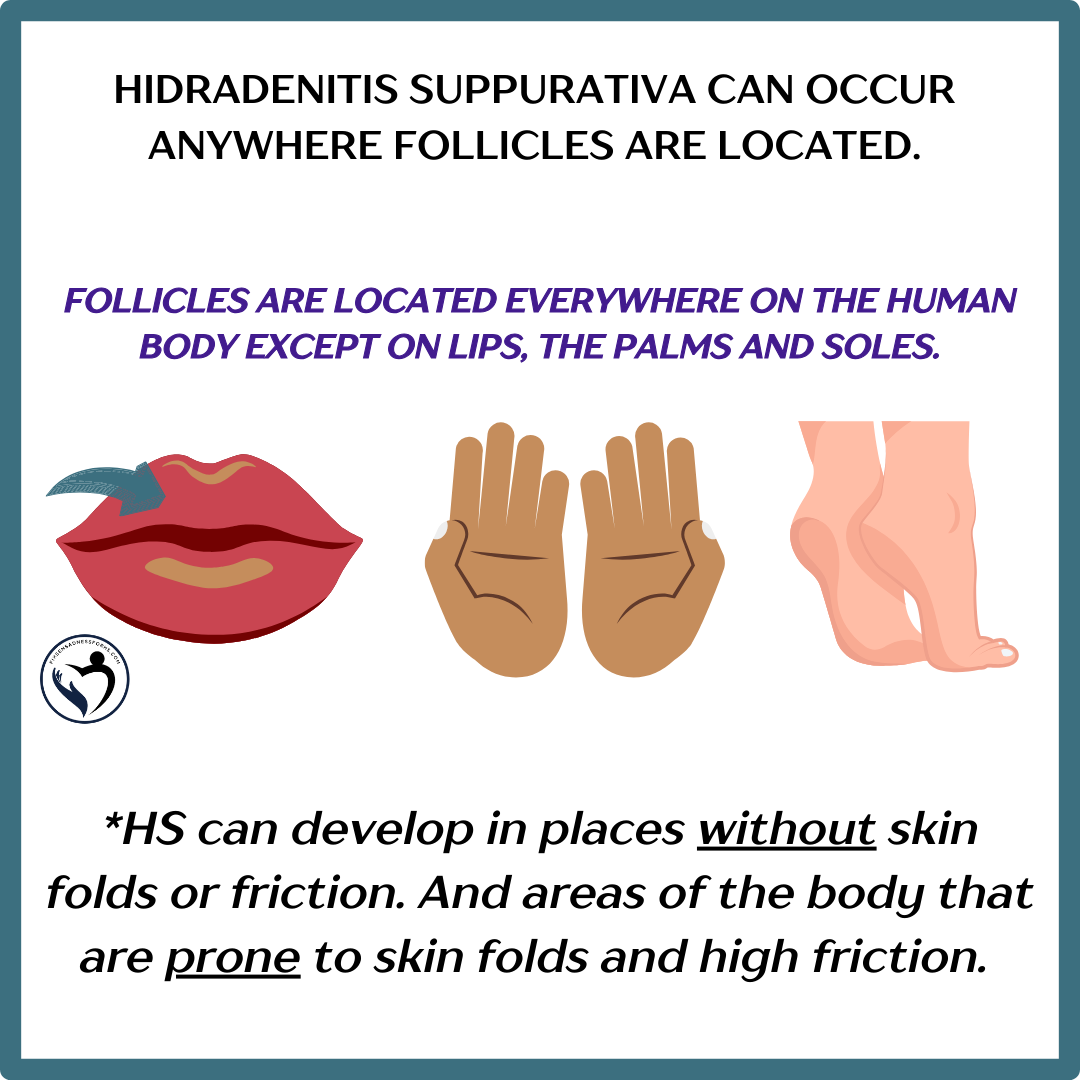
It is possible for HS to occur in the ears and in the nose. HS cannot be developed internally within the body (on organs, intestines, etc.).
There are three stages (III) using the Hurley staging system.
The Hurley staging system is the first staging tool developed for hidradenitis suppurativa by Dr. Harry James Hurley Jr., an American dermatologist, in 1989. And it continues to be a highly utilized tool for assessing HS severity. Across the world.
This tool is used to classify patients with HS into three disease severity groups.
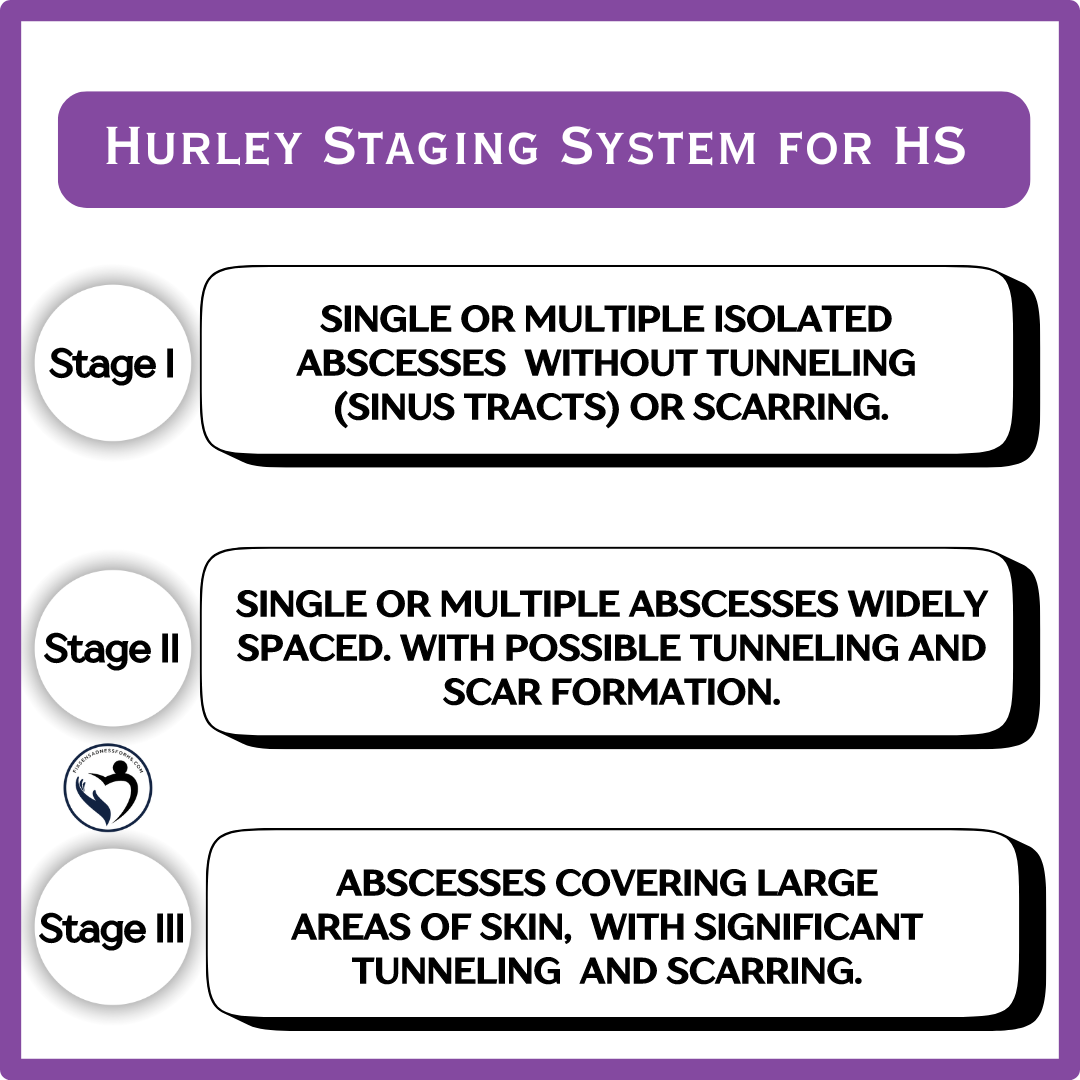
You can have various Hurley stages (I, II, III) on different areas of the body.
HS and the Immune System
It is important for all individuals to be careful when classifying HS as one particular thing or as an unquestionable reality. Research is always ongoing and the complexity of the immune system is truly extraordinary. Our bodies and HS exhibit a great deal of complexity.
What is known HS and the immune:
- HS meets the criteria for a chronic inflammatory illness that has been established.
- But its not that simple
- Research has specifically provided evidence with HS for auto-inflammatory, the innate immune system, and its role in the immune system overreacting.
- HS has never been categorized as an autoimmune condition There is no substantial, long-standing research or pathology that fully meets the criteria. Autoimmune is the adaptive immune system, where healthy tissues are mistakenly identified as foreign and are attacked.
Inserting a big HOWEVER here. Research on HS is always ongoing. The complexity of the immune system is truly extraordinary. Our bodies and HS are very complex. exhibit. Experts may find out there is a place for both auto-inflammatory and autoimmune as they do share common features and overlapping pathways. So don't be surprised if another component is thrown in the mix.
But for the past several years, and for now, chronic inflammatory illness, with a follicular occlusion, microbiome, and biofilm involvement is what long-standing research & pathology supports.
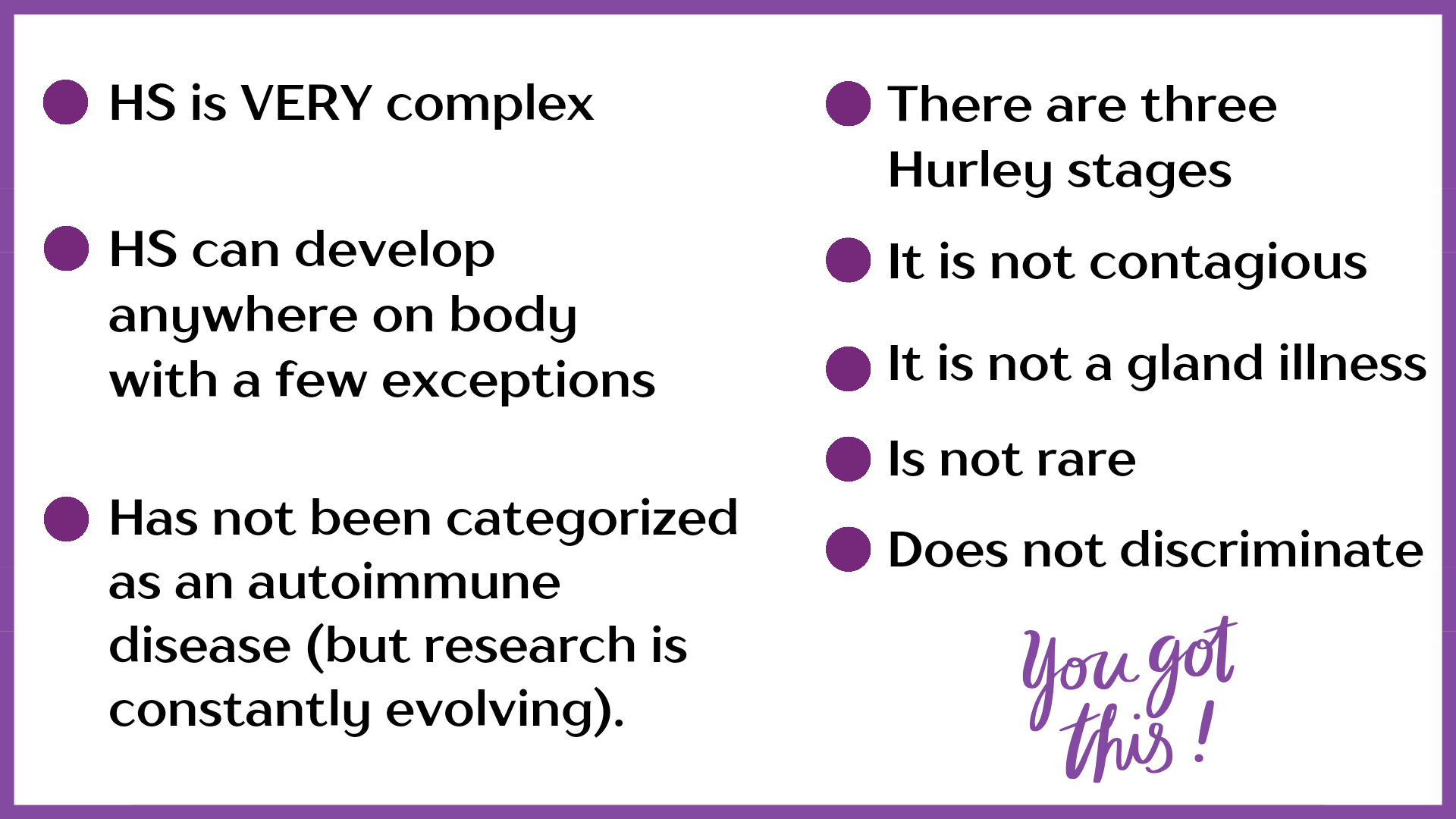
Some Facts:
Throughout the years, below has gained recognition on a large scale.
Here are a few things that are KNOWN:
- The classification of HS as a gland disease was debunked years ago.
- Antibiotics are primarily prescribed for their anti-inflammatory properties unless there is an infection present. If an infection occurs, it is considered a secondary complication. In some cases they are perscribed to keep harmful bacteria at bay (VERY case specific).
- It’s common to have other illnesses or comorbidities, but they don’t change the classification of HS.
- Hidradenitis Suppurativa affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination.
- It is not an infectious illness (not contagious).
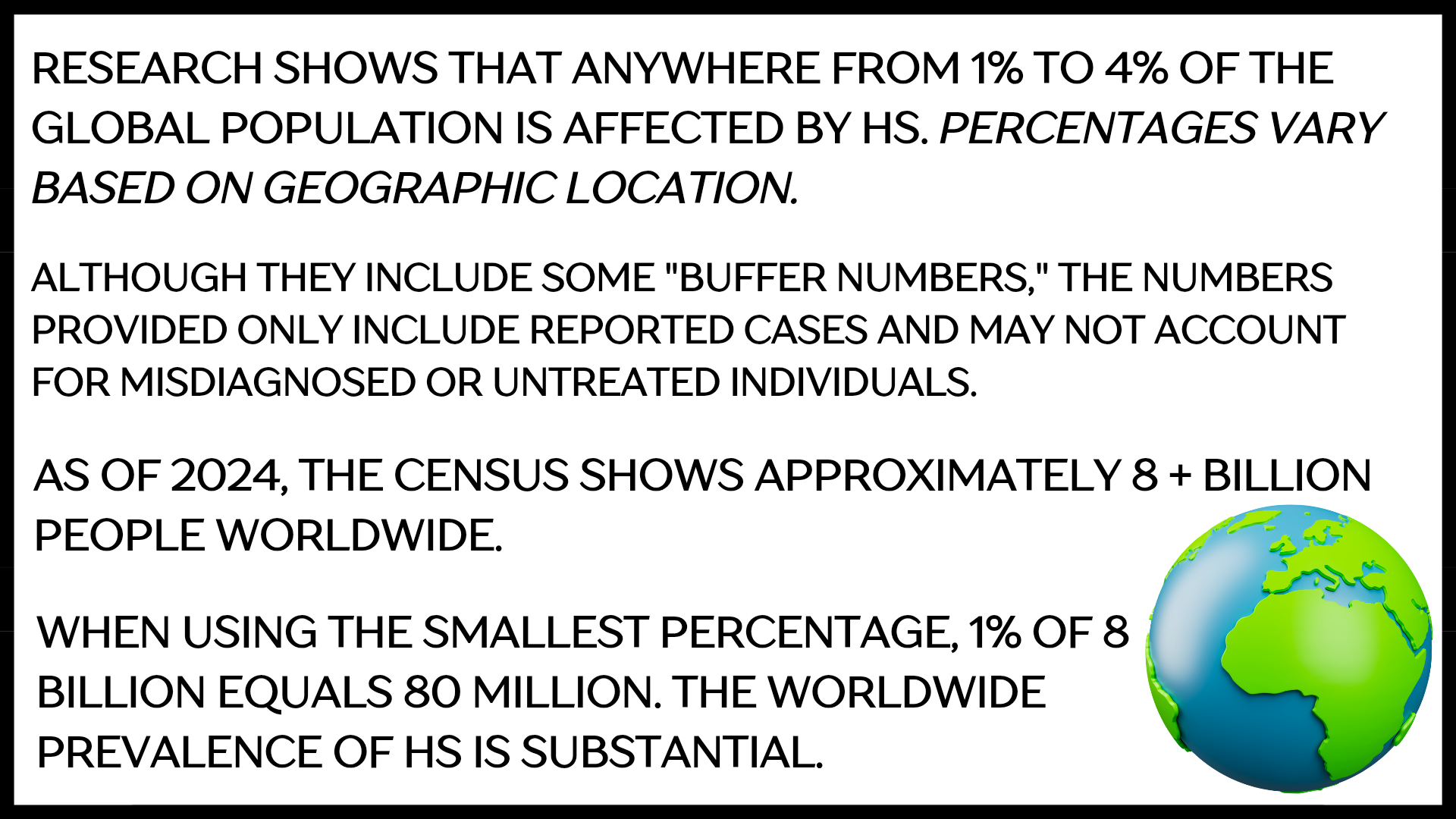
- Is not RARE.
- Putting that into perspective
Misconceptions and Stigmas
These are prevalent in some HS articles, research, online platforms, and support groups. The lack of consistent factual awareness and lack of qualified HS clinicians lead to the ongoing delay in getting a proper diagnosis (is still on average five to seven years).
I will “quote” some of the most common cited misconceptions and stigmas below:
"Where skin rubs together, such as the armpits, groin, buttocks”, and, “HS affects apocrine gland-bearing skin” This statement severely underestimates our illness and is only partially accurate, as you already learned earlier in this article.
"HS is a gland, sweat gland, or infection of the glands”. This is entirely incorrect and correlates directly with the statement above.
Cysts, acne-like, boils, pea-like bumps. For a more precise and informative wording, one can use terms such as abscesses, lesions, or boil-like characteristics (typically used to describe HS that is raised and visible on the skin). Nodules, lumps, and bumps are typically used to describe things beneath the skin.
“HS is more common [fill in blank here]”. Or “HS develops after puberty”. By continuously making these remarks about HS without considering everyone, numerous individuals, including kids, men, and people from all races, are left without any support. Furthermore, full involvement of HS patients in a global study, taking into account race and gender, is necessary for experts to make an informed decision on prevalence.
“HS is rare” Nope. When it comes to HS, it is far from being rare; there are actually millions of individuals worldwide who are afflicted. See previous statement above.
These repetitive statements hinder diagnosis and treatment for many, and exclude thousands in need of support and care.
Quick Recap
Special Note: Researched, compiled, and written by Denise Fixsen. This information is backed by my 46 years of living with Hidradenitis Suppurativa, 10 years of dealing with multiple chronic illnesses, 36 years of advocacy, and continuous education. And to ensure accuracy, reliability, and trustworthiness, I incorporate peer-reviewed studies and other high-quality sources into my articles and material. I also wanted to inform you that I’ve chosen to end my collaboration with editors on my articles. Although there may be grammar errors due to brain illnesses (mostly), with this said, my content remains reliable, factual, and solid.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Sources: PMC7450471, PMID:32884675, doi:10.1001/jamadermatol.2017.0904, doi.org/10.1016/j.clindermatol.2023.08.021, PMC8537933PMID: 34696185, PMC8324042