Research Highlights
Hidradenitis Suppurativa and Risk of Coronary Artery Disease
Research Summery
Topic: Hidradenitis Suppurativa and Risk of Coronary Artery Disease

Method:
A total of 876 articles were identified. After two rounds of independent review by three investigators, seven cohort studies.
The meta-analysis found a significantly elevated risk of both incident and prevalent CAD in patients with HS.
Results:
Overall, 47 CVDs were significantly linked to an increased risk of onset in patients with hidradenitis suppurativa. The greatest risk was for unspecified heart failure, followed by myocardial infarction.
Top 10 CVDs with the Greatest Risk:
•Heart failure, unspecified.
•Old myocardial infarction
•Acute embolism and thrombosis of unspecified deep veins of lower extremity
•Hypertensive heart disease with heart failure
•Pulmonary heart disease and diseases of pulmonary circulation
•Systolic (congestive) heart failure
•Diastolic (congestive) heart failure
•Acute embolism and thrombosis of deep veins of lower extremity
•Pulmonary embolism
Hypertensive heart disease
Conclusion:
The current systematic review and meta-analysis found a significantly increased risk of both prevalent and incident CAD among patients with HS.
The results of this study clearly indicate the need for a holistic approach to patients with [hidradenitis suppurativa] and the necessity of close cooperation between dermatologists and cardiologists,” investigators concluded. “Prophylaxis of CVD should be introduced in all [hidradenitis suppurativa] patients; they should be closely monitored and treated before developing life-threatening conditions.
Cited Research:
Special Note:
Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the skin, immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Topic: Hidradenitis Suppurativa and Risk of Coronary Artery Disease

Method:
A total of 876 articles were identified. After two rounds of independent review by three investigators, seven cohort studies.
The meta-analysis found a significantly elevated risk of both incident and prevalent CAD in patients with HS.
Results:
Overall, 47 CVDs were significantly linked to an increased risk of onset in patients with hidradenitis suppurativa. The greatest risk was for unspecified heart failure, followed by myocardial infarction.
Top 10 CVDs with the Greatest Risk:
•Heart failure, unspecified.
•Old myocardial infarction
•Acute embolism and thrombosis of unspecified deep veins of lower extremity
•Hypertensive heart disease with heart failure
•Pulmonary heart disease and diseases of pulmonary circulation
•Systolic (congestive) heart failure
•Diastolic (congestive) heart failure
•Acute embolism and thrombosis of deep veins of lower extremity
•Pulmonary embolism
Hypertensive heart disease
Conclusion:
The current systematic review and meta-analysis found a significantly increased risk of both prevalent and incident CAD among patients with HS.
The results of this study clearly indicate the need for a holistic approach to patients with [hidradenitis suppurativa] and the necessity of close cooperation between dermatologists and cardiologists,” investigators concluded. “Prophylaxis of CVD should be introduced in all [hidradenitis suppurativa] patients; they should be closely monitored and treated before developing life-threatening conditions.
Cited Research:
- Hidradenitis Suppurativa and Risk of Coronary Artery Disease: A Systematic Review and Meta-Analysis: See Here
- Hidradenitis Suppurativa Linked to Increased Risk of Cardiovascular Diseases: See Here
- Early impairment of endothelial and myocardial function in patients with hidradenitis suppurativa: See Here
Special Note:
Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the skin, immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Itching (pruritus) with Hidradenitis Suppurativa
Research Summary
Topic: Itching (pruritus) with Hidradenitis Suppurativa
Method:
Twenty different articles were selected for the study.
Results:
Itching, or pruritus, is a common and bothersome symptom of hidradenitis suppurativa (HS), affecting between 62% and 75% of people with the condition.
Conclusion:
Despite a lack of complete understanding of itch in HS, it is an important aspect of the disease, reported in 62% to 75% of patients. Further study to gain a better understanding of the etiopathogenesis and optimal therapeutic modalities for itch in HS will allow clinicians to better address this aspect of the disease and reduce its impact on quality of life.
Itchiness associated with HS may be caused by the release of histamine from mast cells in the nodules, abscesses, and surrounding skin. This histamine release can cause itching and other allergic symptoms.
Cited Research:
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the skin, immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Topic: Itching (pruritus) with Hidradenitis Suppurativa
Method:
Twenty different articles were selected for the study.
Results:
Itching, or pruritus, is a common and bothersome symptom of hidradenitis suppurativa (HS), affecting between 62% and 75% of people with the condition.
Conclusion:
Despite a lack of complete understanding of itch in HS, it is an important aspect of the disease, reported in 62% to 75% of patients. Further study to gain a better understanding of the etiopathogenesis and optimal therapeutic modalities for itch in HS will allow clinicians to better address this aspect of the disease and reduce its impact on quality of life.
Itchiness associated with HS may be caused by the release of histamine from mast cells in the nodules, abscesses, and surrounding skin. This histamine release can cause itching and other allergic symptoms.
Cited Research:
- Itch in Hidradenitis Suppurativa/Acne Inversa: A Systematic Review:
See Here - Pruritus and Malodour in Patients with Hidradenitis Suppurativa: Impact on Quality of Life and Clinical Features Associated with Symptom Severity: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the skin, immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Hidradenitis Suppurativa and Diabetes Mellitus
Research Summary
Topic: Hidradenitis Suppurativa and Diabetes Mellitus
Method:
A systematic review and meta-analysis. The systematic review included 107,050 patients from 14 studies; the meta-analysis included 104,373 patients from 7 studies. On the basis of meta-analysis, the prevalence of diabetes mellitus was 10.6% in patients with hidradenitis suppurativa and 3.8% in patients without hidradenitis suppurativa.
Results:
Compared with the general population, patients with hidradenitis suppurativa were nearly 3 times more likely to have diabetes mellitus.
Conclusion:
Hidradenitis suppurativa is significantly associated with an increased prevalence of diabetes mellitus.
Cited Research:
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-19-2024
Topic: Hidradenitis Suppurativa and Diabetes Mellitus
Method:
A systematic review and meta-analysis. The systematic review included 107,050 patients from 14 studies; the meta-analysis included 104,373 patients from 7 studies. On the basis of meta-analysis, the prevalence of diabetes mellitus was 10.6% in patients with hidradenitis suppurativa and 3.8% in patients without hidradenitis suppurativa.
Results:
Compared with the general population, patients with hidradenitis suppurativa were nearly 3 times more likely to have diabetes mellitus.
Conclusion:
Hidradenitis suppurativa is significantly associated with an increased prevalence of diabetes mellitus.
Cited Research:
- Hidradenitis suppurativa and diabetes mellitus: A systematic review and meta-analysis: See Here
- Screening for Diabetes Mellitus in Patients with Hidradenitis Suppurativa—A Monocentric Study in Germany: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-19-2024
Association Between Hidradenitis Suppurativa and Metabolic Syndrome (MetS).
Research Summary
Topic:
The association of the metabolic syndrome (MetS) and its components with immune-mediated chronic inflammatory disorders (like HS). The association of the metabolic syndrome (MetS) and its components with immune-mediated chronic inflammatory disorders (like HS) has attracted much interest within the last two decades. Although solid data support the association between HS and MetS, the consequences of this relationship have only recently been studied.
Methods:
A systematic review and meta-analysis of observational studies on HS and MetS in adults. MEDLINE, SCOPUS, SCIELO, Google Scholar, Science Direct, and LILACS from the inception of the databases to January 2016. A subgroup analysis was related to the type of HS patient (general patients vs hospital patients) and age group (adults vs children and adults).
Results:
Five studies including 3950 HS patients were analyzed. We found that MetS was pres-ent in 9.64% of HS patients. Studies from tertiary care hospital dermatology clinics reported a greater risk for MetS than studies carried out in patients treated outside hospitals. Studies that included pediatric populations reported a significant association.
Conclusion:
HS patients have an increased risk for MetS. Clinicians should consider screening HS patients for metabolic risk factors.
Cited Research:
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Topic:
The association of the metabolic syndrome (MetS) and its components with immune-mediated chronic inflammatory disorders (like HS). The association of the metabolic syndrome (MetS) and its components with immune-mediated chronic inflammatory disorders (like HS) has attracted much interest within the last two decades. Although solid data support the association between HS and MetS, the consequences of this relationship have only recently been studied.
Methods:
A systematic review and meta-analysis of observational studies on HS and MetS in adults. MEDLINE, SCOPUS, SCIELO, Google Scholar, Science Direct, and LILACS from the inception of the databases to January 2016. A subgroup analysis was related to the type of HS patient (general patients vs hospital patients) and age group (adults vs children and adults).
Results:
Five studies including 3950 HS patients were analyzed. We found that MetS was pres-ent in 9.64% of HS patients. Studies from tertiary care hospital dermatology clinics reported a greater risk for MetS than studies carried out in patients treated outside hospitals. Studies that included pediatric populations reported a significant association.
Conclusion:
HS patients have an increased risk for MetS. Clinicians should consider screening HS patients for metabolic risk factors.
Cited Research:
- Metabolic syndrome and hidradenitis suppurativa: epidemiological, molecular, and therapeutic aspects: See Here
- Hidradenitis suppurativa and the metabolic syndrome: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Hidradenitis Suppurativa & Polycystic Ovary Syndrome (PCOS)
Research Summary
Topic: Hidradenitis Suppurativa & Polycystic Ovary Syndrome (PCOS)
Method:
A Population Based Analysis in the United States. In a cross-sectional analysis involving 22,990 patients with HS using clinical data from a multihealth system. More than 55 million unique patients across all census regions of the United States.
Results:
The prevalence of PCOS among patients with HS was 9.0%, compared with 2.9% in patients without HS.
Conclusion:
In summary, pooled analysis of existing case-control studies supports a significant association between hidradenitis suppurativa and polycystic ovarian syndrome.
*However, the findings suggest that PCOS does not forecast a worsening prognosis in the severity of HS.
Cited Research:
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Topic: Hidradenitis Suppurativa & Polycystic Ovary Syndrome (PCOS)
Method:
A Population Based Analysis in the United States. In a cross-sectional analysis involving 22,990 patients with HS using clinical data from a multihealth system. More than 55 million unique patients across all census regions of the United States.
Results:
The prevalence of PCOS among patients with HS was 9.0%, compared with 2.9% in patients without HS.
Conclusion:
In summary, pooled analysis of existing case-control studies supports a significant association between hidradenitis suppurativa and polycystic ovarian syndrome.
*However, the findings suggest that PCOS does not forecast a worsening prognosis in the severity of HS.
Cited Research:
- Hidradenitis suppurativa and polycystic ovarian syndrome: Systematic review and meta-analysis:
See Here - Hidradenitis Suppurativa Is Associated with Polycystic Ovary Syndrome: A Population-Based Analysis in the United States:
See Here - Polycystic ovary syndrome not associated with hidradenitis suppurativa severity: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
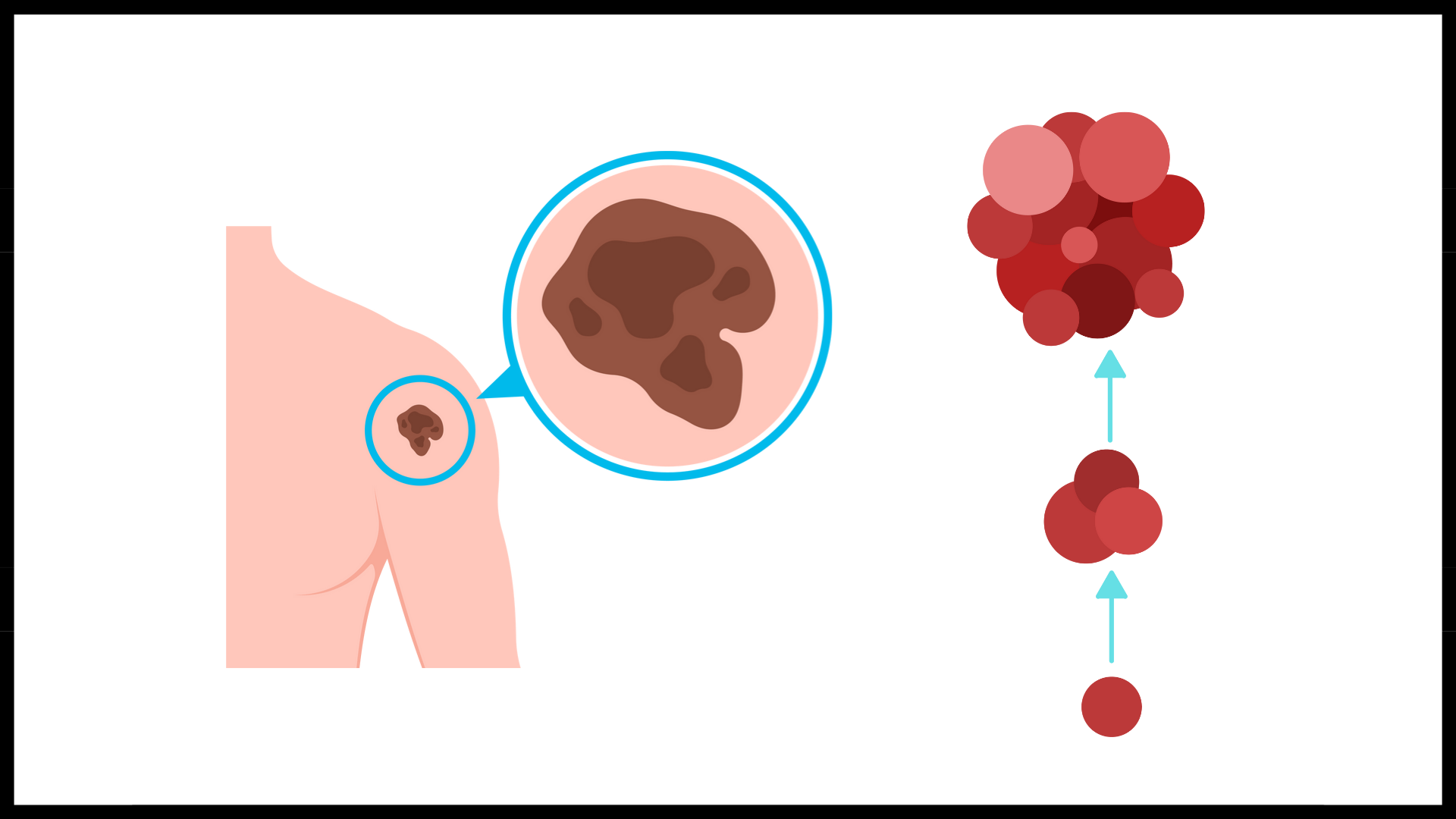
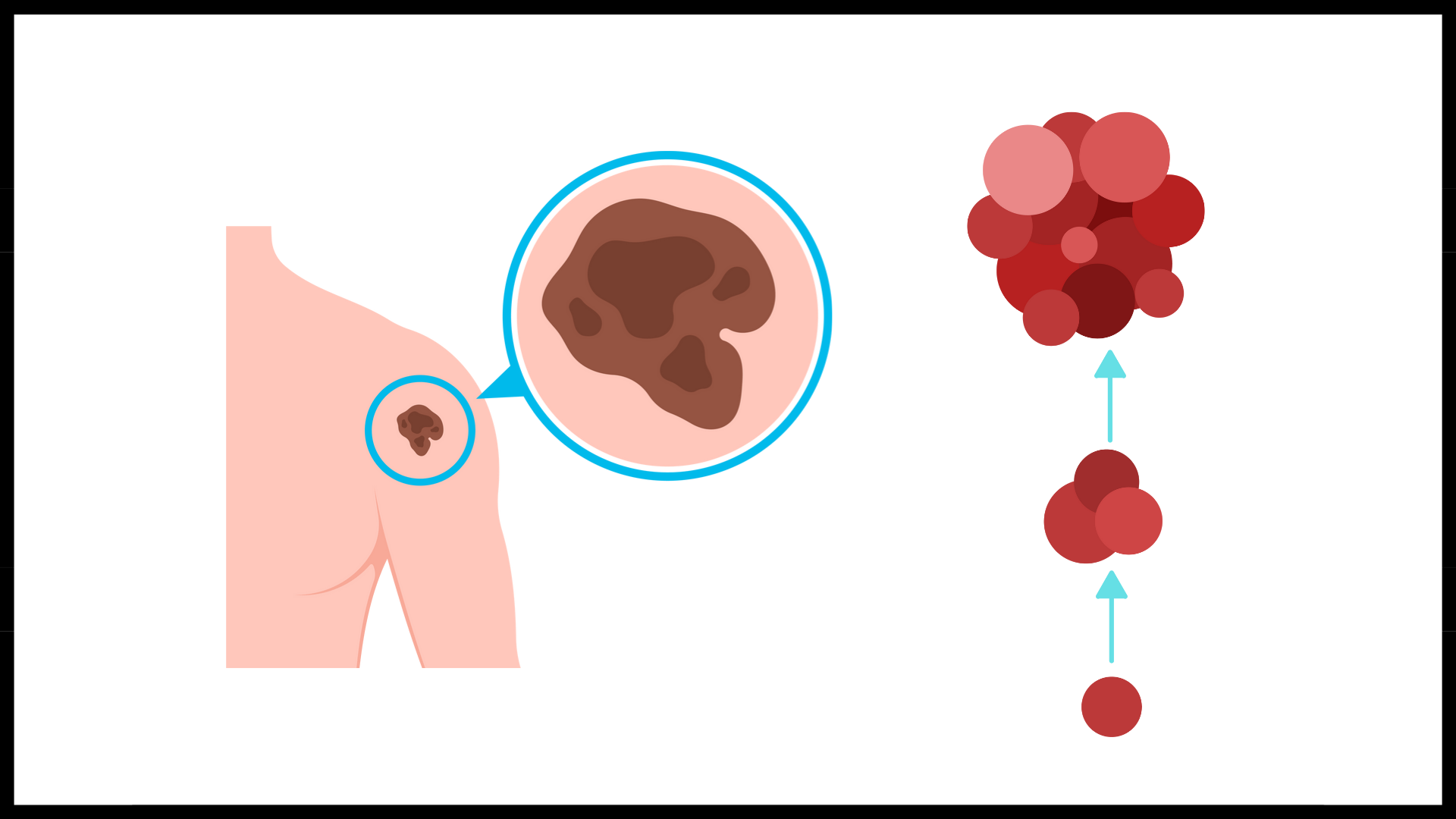
Hidradenitis Suppurativa And Increased Risk Of Overall Cancer
Research Summery
Topic: Hidradenitis Suppurativa And Increased Risk Of Overall Cancer
Method:
A population-based study of 22,468 patients with hidradenitis suppurativa in the Republic of Korea. And a cross-sectional cohort analysis used standardized electronic health record information database for 55 million patients from 27 integrated health systems across the United States.
Results:
The studies showed HS to be associated with a significantly increased risk of overall cancer as well as several specific cancers such as; Hodgkin lymphoma, oral, pharyngeal, central nervous system, liver, nonmelanoma skin, prostate, and colorectal cancer.
Additionally, over the past several years, research has consistently found a link between HS and nonmelanoma skin cancers, including squamous cell carcinoma and basal cell carcinoma.
Conclusion:
Hidradenitis suppurativa appears to be associated with an overall risk of cancer and several specific cancers, such as OCPC, nonmelanoma skin cancer, CNS cancer, colorectal cancer, and prostate cancer. More intense cancer surveillance may be warranted in patients with HS. For early detection of skin cancer, more aggressive histologic examination and a high level of suspicion are required. Lifestyle modifications in patients with HS to address behaviors such as smoking or alcohol use or conditions such as obesity should be emphasized. If patients develop any signs or symptoms suggesting Hodgkin lymphoma, such as painless lymphadenopathy, persistent fatigue, unexplained fever, night sweats, or unexplained weight loss, more aggressive laboratory testing, imaging studies, and histologic examinations are recommended, especially in men with HS. Studies on various ethnic groups to evaluate the risk of cancer in patients with HS are needed.
The studies suggest that the most significant risk factors in HS patients are sex (males), long HS duration time, perianal/gluteal region, and Hurley Stage III. Considering the high mortality rate (40%), we suggest screening/examining SCC lesions in all HS patients for SCC. The potential risk factors such as males, Hurley Stage III, long HS duration time, and location of HS in the perianal/gluteal region should be considered. As HS is a chronic skin disease with the possibility of SCC occurring in these lesions, we should be encouraged to adopt surgical rather than conservative dermatological treatment.
Cited Research:
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Topic: Hidradenitis Suppurativa And Increased Risk Of Overall Cancer
Method:
A population-based study of 22,468 patients with hidradenitis suppurativa in the Republic of Korea. And a cross-sectional cohort analysis used standardized electronic health record information database for 55 million patients from 27 integrated health systems across the United States.
Results:
The studies showed HS to be associated with a significantly increased risk of overall cancer as well as several specific cancers such as; Hodgkin lymphoma, oral, pharyngeal, central nervous system, liver, nonmelanoma skin, prostate, and colorectal cancer.
Additionally, over the past several years, research has consistently found a link between HS and nonmelanoma skin cancers, including squamous cell carcinoma and basal cell carcinoma.
Conclusion:
Hidradenitis suppurativa appears to be associated with an overall risk of cancer and several specific cancers, such as OCPC, nonmelanoma skin cancer, CNS cancer, colorectal cancer, and prostate cancer. More intense cancer surveillance may be warranted in patients with HS. For early detection of skin cancer, more aggressive histologic examination and a high level of suspicion are required. Lifestyle modifications in patients with HS to address behaviors such as smoking or alcohol use or conditions such as obesity should be emphasized. If patients develop any signs or symptoms suggesting Hodgkin lymphoma, such as painless lymphadenopathy, persistent fatigue, unexplained fever, night sweats, or unexplained weight loss, more aggressive laboratory testing, imaging studies, and histologic examinations are recommended, especially in men with HS. Studies on various ethnic groups to evaluate the risk of cancer in patients with HS are needed.
The studies suggest that the most significant risk factors in HS patients are sex (males), long HS duration time, perianal/gluteal region, and Hurley Stage III. Considering the high mortality rate (40%), we suggest screening/examining SCC lesions in all HS patients for SCC. The potential risk factors such as males, Hurley Stage III, long HS duration time, and location of HS in the perianal/gluteal region should be considered. As HS is a chronic skin disease with the possibility of SCC occurring in these lesions, we should be encouraged to adopt surgical rather than conservative dermatological treatment.
Cited Research:
- Assessment of Overall and Specific Cancer Risks in Patients With Hidradenitis Suppurativa: See Here
- Hidradenitis suppurativa and squamous cell carcinoma: a systematic review of the literature: See Here
- Association Between Hidradenitis Suppurativa and Lymphoma: See Here
- Risk of keratinocyte carcinoma among patients with hidradenitis suppurativa: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Impact of Pregnancy on Hidradenitis Suppurativa
Research Summary
Topic: Impact of Pregnancy on Hidradenitis Suppurativa
Methods:
The PubMed and Embase databases were systematically searched for relevant articles from database inception until November 22, 2020. The inclusion criteria were a study population with the diagnosis of HS and discussion of pregnancy impact on the HS disease course or postpartum flare. Study characteristics, patient demographics, HS severity, and HS disease course during pregnancy and the postpartum period were extracted by 2 independent reviewers. The primary study outcome was the pooled odds ratio of improvement or of worsening of HS disease activity during.
Results:
The systematic search identified 8 studies for analysis. There was a total of 672 cases for which data on the patient-reported HS disease course during pregnancy were available, and 164 cases for which data on patient-reported postpartum flare were available. In the meta-analyses, the rate of HS disease improvement was 24% and the rate of HS disease worsening was 20%. Sixty percent of patients experienced a postpartum flare.
Conclusion:
While about a quarter of women experienced improvement in HS during pregnancy, the majority had a stable or worsened disease course, and over half of patients experienced a postpartum flare. Close monitoring of HS patients is needed during pregnancy and postpartum periods, as patients may need continued, or even escalated, disease management.
Cited Research:
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Topic: Impact of Pregnancy on Hidradenitis Suppurativa
Methods:
The PubMed and Embase databases were systematically searched for relevant articles from database inception until November 22, 2020. The inclusion criteria were a study population with the diagnosis of HS and discussion of pregnancy impact on the HS disease course or postpartum flare. Study characteristics, patient demographics, HS severity, and HS disease course during pregnancy and the postpartum period were extracted by 2 independent reviewers. The primary study outcome was the pooled odds ratio of improvement or of worsening of HS disease activity during.
Results:
The systematic search identified 8 studies for analysis. There was a total of 672 cases for which data on the patient-reported HS disease course during pregnancy were available, and 164 cases for which data on patient-reported postpartum flare were available. In the meta-analyses, the rate of HS disease improvement was 24% and the rate of HS disease worsening was 20%. Sixty percent of patients experienced a postpartum flare.
Conclusion:
While about a quarter of women experienced improvement in HS during pregnancy, the majority had a stable or worsened disease course, and over half of patients experienced a postpartum flare. Close monitoring of HS patients is needed during pregnancy and postpartum periods, as patients may need continued, or even escalated, disease management.
Cited Research:
- Impact of Pregnancy on Hidradenitis Suppurativa Disease Course: A Systematic Review and Meta-Analysis: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
African Americans may be a significant risk factor for having more severe Hidradenitis Suppurativa
Research Summary
Topic: African Americans may be a significant risk factor for having more severe Hidradenitis Suppurativa

Methods:
We reviewed 1190 patients seen at the Medical College of Wisconsin with ≥3 encounters for HS between 1/1/2002 and 3/19/2019, excluding those without race data or an encounter in which HS was treated.
Results:
A total of 953 patients were included; 470 patients were Black or African American non-Hispanic, 39 Hispanic, 418 White non-Hispanic, and 26 other race or ethnicity. Black patients had 2.8 times the odds of having Hurley stage III disease, 2.86 times the risk for experiencing an ED visit for HS, 2.25 times the risk for experiencing a hospitalization for HS, and 1.61 times the risk for experiencing a surgical encounter for HS when compared to White patients.
Conclusion:
African Americans face significant disparities in HS severity. The causes of these disparities must be further investigated and addressed.
Note:
"There are several confounding factors including higher rates metabolic syndrome in African Americans".
“Rigorous studies on access to and utilization of care and treatments for HS in African Americans are sorely needed, while large-scale genetic studies may be warranted to fully investigate the possibility of a genetic predisposition for severe and uncontrolled HS in African Americans.”
Cited Research:
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Topic: African Americans may be a significant risk factor for having more severe Hidradenitis Suppurativa

Methods:
We reviewed 1190 patients seen at the Medical College of Wisconsin with ≥3 encounters for HS between 1/1/2002 and 3/19/2019, excluding those without race data or an encounter in which HS was treated.
Results:
A total of 953 patients were included; 470 patients were Black or African American non-Hispanic, 39 Hispanic, 418 White non-Hispanic, and 26 other race or ethnicity. Black patients had 2.8 times the odds of having Hurley stage III disease, 2.86 times the risk for experiencing an ED visit for HS, 2.25 times the risk for experiencing a hospitalization for HS, and 1.61 times the risk for experiencing a surgical encounter for HS when compared to White patients.
Conclusion:
African Americans face significant disparities in HS severity. The causes of these disparities must be further investigated and addressed.
Note:
"There are several confounding factors including higher rates metabolic syndrome in African Americans".
“Rigorous studies on access to and utilization of care and treatments for HS in African Americans are sorely needed, while large-scale genetic studies may be warranted to fully investigate the possibility of a genetic predisposition for severe and uncontrolled HS in African Americans.”
Cited Research:
- African American race is a risk factor for severe hidradenitis suppurativa:
See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Inflammatory Arthritis among Hidradenitis Suppurativa
Research Summery
Topic: Inflammatory Arthritis among Hidradenitis Suppurativa

Method:
Seven studies were entered in the analysis, with 200,361 HS patients and 385,599 controls.
Results:
Pooled analysis illustrated a significantly increased risk of inflammatory arthritis in HS patients compared to controls. There was also a statistically significant association between HS and spondyloarthritis, and between HS and AS. Moreover, pooled analysis showed a statistically significant association between HS and RA.
Conclusion:
Our findings show that HS patients have a 3-fold increased risk of developing inflammatory arthritis. HS patients are specifically at a higher risk for spondyloarthritis, its subtype AS, and RA.
Cited Research:
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Topic: Inflammatory Arthritis among Hidradenitis Suppurativa

Method:
Seven studies were entered in the analysis, with 200,361 HS patients and 385,599 controls.
Results:
Pooled analysis illustrated a significantly increased risk of inflammatory arthritis in HS patients compared to controls. There was also a statistically significant association between HS and spondyloarthritis, and between HS and AS. Moreover, pooled analysis showed a statistically significant association between HS and RA.
Conclusion:
Our findings show that HS patients have a 3-fold increased risk of developing inflammatory arthritis. HS patients are specifically at a higher risk for spondyloarthritis, its subtype AS, and RA.
Cited Research:
- Association between Hidradenitis Suppurativa and Inflammatory Arthritis: A Systematic Review and Meta-Analysis: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Fatigue is associated with disease severity in adult patients with Hidradenitis Suppurativa
Research Summery
Topic: To examine the possible association between HS severity and fatigue and identify fatigue subtypes present in patients with HS.

Method:
Data from 654 adult patients with HS were analysed and compared with 3,788 reference individuals from the general population.
Total and subtype fatigue scores for patients with HS were significantly higher compared with the general population reference individuals and increased with higher HS severity, itch, pain, sleep, dermatology life quality index scores and lower socioeconomic status.
Results:
Data from 654 adult patients with HS were analysed and compared with 3,788 reference individuals from the general population.
Total and subtype fatigue scores for patients with HS were significantly higher compared with the general population reference individuals and increased with higher HS severity, itch, pain, sleep, dermatology life quality index scores and lower socioeconomic status.
The association between HS severity and increased fatigue scores remained statistically significant after adjustment for age, sex, and socioeconomic status.
Conclusion:
Patients with HS had a significantly higher fatigue score compared with the general population reference individuals in a severity-dependent manner. A higher awareness of fatigue as a symptom in patients with HS is warranted.
Cited Research:
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-19-2024
Topic: To examine the possible association between HS severity and fatigue and identify fatigue subtypes present in patients with HS.

Method:
Data from 654 adult patients with HS were analysed and compared with 3,788 reference individuals from the general population.
Total and subtype fatigue scores for patients with HS were significantly higher compared with the general population reference individuals and increased with higher HS severity, itch, pain, sleep, dermatology life quality index scores and lower socioeconomic status.
Results:
Data from 654 adult patients with HS were analysed and compared with 3,788 reference individuals from the general population.
Total and subtype fatigue scores for patients with HS were significantly higher compared with the general population reference individuals and increased with higher HS severity, itch, pain, sleep, dermatology life quality index scores and lower socioeconomic status.
The association between HS severity and increased fatigue scores remained statistically significant after adjustment for age, sex, and socioeconomic status.
Conclusion:
Patients with HS had a significantly higher fatigue score compared with the general population reference individuals in a severity-dependent manner. A higher awareness of fatigue as a symptom in patients with HS is warranted.
Cited Research:
- Fatigue is associated with disease severity in adult patients with hidradenitis suppurativa: See Here
- Fatigue in chronic inflammation - a link to pain pathways: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-19-2024
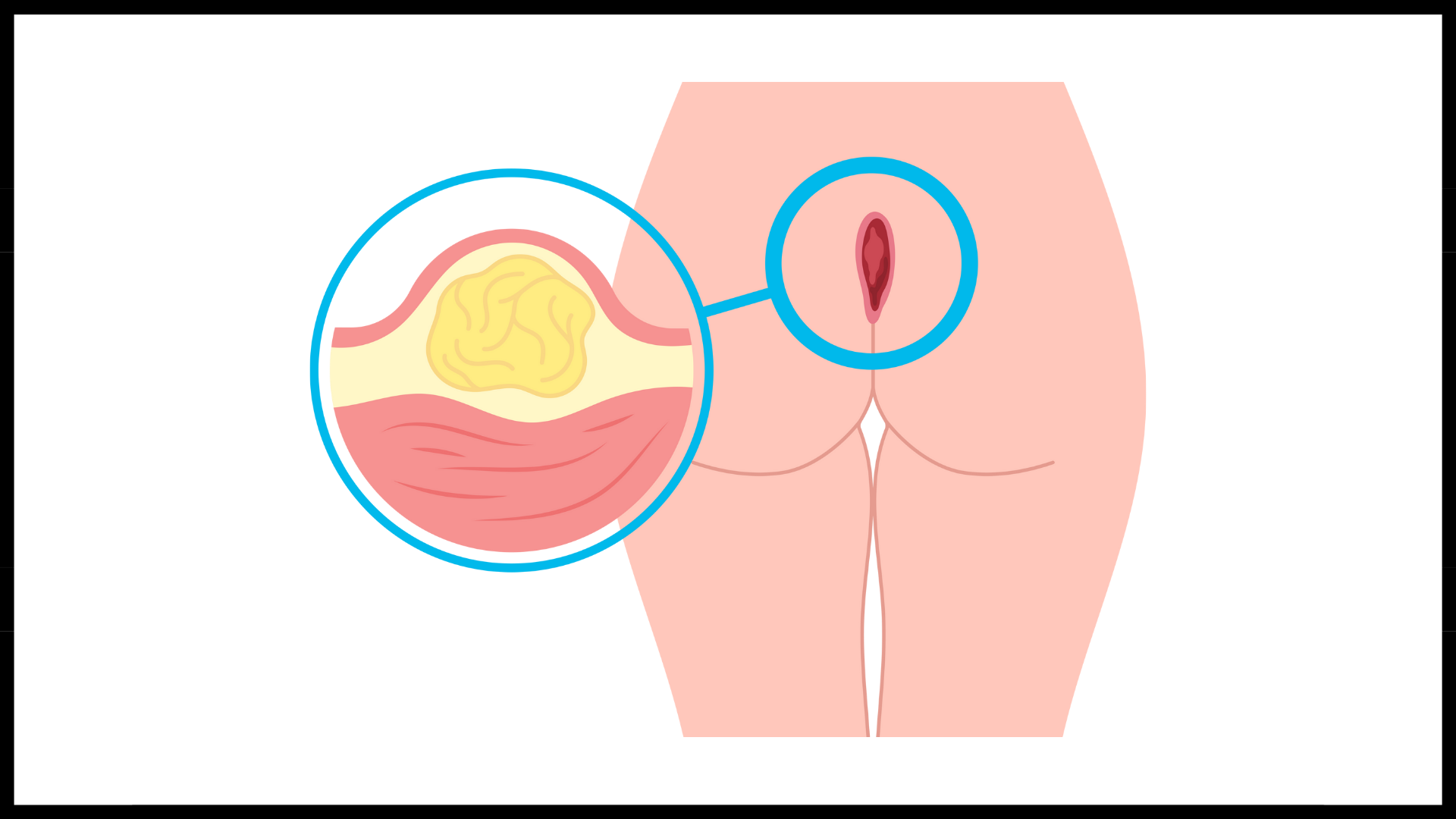
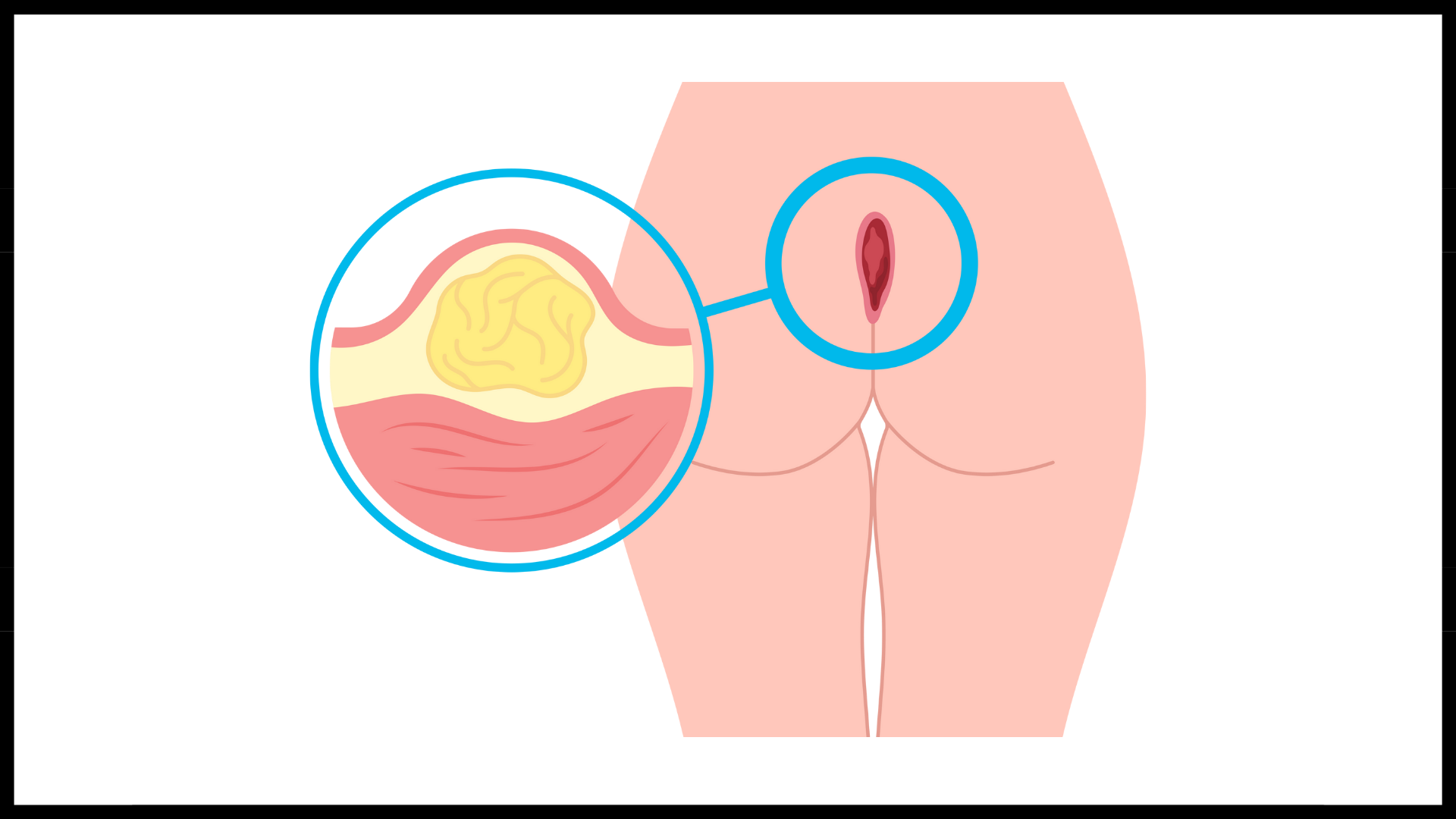
Pilonidal disease (PD) or Pilonidal sinus disease (PSD)
Research Summery
Topic: Pilonidal disease (PD) or Pilonidal sinus disease (PSD)
Methods:
A total of 839 patients with HS were included in the study; the inflammatory HS phenotype was the most common.
Results:
Of the subjects, 530 presented Hurley stage II or III. PSD was present in 269 of the patients.
In an international multicentre retrospective cross-sectional study based on data collection from a large cohort of patients with HS with and without histopathology. From a total of 2465 patients with HS included in the study, 661 reported lesions in the IG area. Of the 238 patients with an available clinical diagnosis, PSD was diagnosed in 186 patients.
Conclusion:
The high prevalence of PSD suggests a strong link with HS. Therefore, it may be useful to identify common pathophysiological mechanisms and develop common therapeutic strategies. Pilonidal sinus disease is the most frequent comorbidity in patients with hidradenitis suppurativa. The results suggest that pilonidal sinus disease and elapsed time between pilonidal sinus disease and hidradenitis suppurativa diagnosis could be risk markers for hidradenitis suppurativa severity.
Pilonidal disease (PD) or Pilonidal sinus disease (PSD) - This is a dermatological soft tissue process that is relatively common and affects both the pediatric population and adults. It is associated with several misconceptions.
PD typically occurs in the sacrococcygeal regions (tailbone, sacrum, and coccyx).
Although less common, researchers have reported PD in other parts of the body, such as:
•Scalp
•Nose
•Abdomen
•Neck
•Arm Pit
•Groin
•Vulva
•Clitoris
•Penis
•Hand
•Spaces between fingers & toes
•Around fingernails & toenails
*Pilonidal cysts and sinuses are a spectrum of pilonidal disease conditions.
Cited Research:
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and does not discriminate. Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Topic: Pilonidal disease (PD) or Pilonidal sinus disease (PSD)
Methods:
A total of 839 patients with HS were included in the study; the inflammatory HS phenotype was the most common.
Results:
Of the subjects, 530 presented Hurley stage II or III. PSD was present in 269 of the patients.
In an international multicentre retrospective cross-sectional study based on data collection from a large cohort of patients with HS with and without histopathology. From a total of 2465 patients with HS included in the study, 661 reported lesions in the IG area. Of the 238 patients with an available clinical diagnosis, PSD was diagnosed in 186 patients.
Conclusion:
The high prevalence of PSD suggests a strong link with HS. Therefore, it may be useful to identify common pathophysiological mechanisms and develop common therapeutic strategies. Pilonidal sinus disease is the most frequent comorbidity in patients with hidradenitis suppurativa. The results suggest that pilonidal sinus disease and elapsed time between pilonidal sinus disease and hidradenitis suppurativa diagnosis could be risk markers for hidradenitis suppurativa severity.
Pilonidal disease (PD) or Pilonidal sinus disease (PSD) - This is a dermatological soft tissue process that is relatively common and affects both the pediatric population and adults. It is associated with several misconceptions.
PD typically occurs in the sacrococcygeal regions (tailbone, sacrum, and coccyx).
Although less common, researchers have reported PD in other parts of the body, such as:
•Scalp
•Nose
•Abdomen
•Neck
•Arm Pit
•Groin
•Vulva
•Clitoris
•Penis
•Hand
•Spaces between fingers & toes
•Around fingernails & toenails
*Pilonidal cysts and sinuses are a spectrum of pilonidal disease conditions.
Cited Research:
- Pilonidal sinus disease: an intergluteal localization of hidradenitis suppurativa/acne inversa: a cross-sectional study among 2465 patients: See Here
- Pilonidal Sinus Disease is Associated with Severe Hidradenitis Suppurativa in a Spanish Cohort: See Here
- Rethinking the causes of pilonidal sinus disease: a matched cohort study: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and does not discriminate. Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
The Association between Hidradenitis Suppurativa and Abnormalities in Semen Parameters and Male Sexual Function
Research Summery
Topic: The Association between Hidradenitis Suppurativa and Abnormalities in Semen Parameters and Male Sexual Function

Method:
This study comprehensively evaluated the association of HS with spermatogenesis and male sexual function using semen analysis, testicular Doppler ultrasound, the IIEF-15 questionnaire, and hormonal and endocrine profiles. Patients with HS involving the gluteal-genital area had significantly reduced semen parameters compared with the remaining patients with HS and healthy men.
Results:
Both HS and male infertility are associated with impaired quality of life, sexual dysfunction, and poor general health, including higher-than-normal rates of cardiovascular diseases, diabetes, and mental health disorders (1, 8‒11).
Thus, the systemic and local inflammation involving the perineal area in HS could contribute to male infertility (1, 2).
The study found significant sexual dysfunction and decreased semen parameters in young men with hidradenitis suppurativa, specifically when the gluteal-genital area was involved. Therefore, fertility and sexual function should be evaluated as part of the management of these patients, and when relevant, semen cryopreservation should be discussed. These findings should prompt further research toward implementing a standard of care.
Conclusion:
The association between HS in reproductive-age men and impaired semen parameters and sexual function has considerable clinical relevance. These findings suggest that fertility and sexual function should be routinely assessed as part of the multidisciplinary management of HS in young men, specifically those with gluteal and genital lesions.
Cited Research:
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and does not discriminate. Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
Topic: The Association between Hidradenitis Suppurativa and Abnormalities in Semen Parameters and Male Sexual Function

Method:
This study comprehensively evaluated the association of HS with spermatogenesis and male sexual function using semen analysis, testicular Doppler ultrasound, the IIEF-15 questionnaire, and hormonal and endocrine profiles. Patients with HS involving the gluteal-genital area had significantly reduced semen parameters compared with the remaining patients with HS and healthy men.
Results:
Both HS and male infertility are associated with impaired quality of life, sexual dysfunction, and poor general health, including higher-than-normal rates of cardiovascular diseases, diabetes, and mental health disorders (1, 8‒11).
Thus, the systemic and local inflammation involving the perineal area in HS could contribute to male infertility (1, 2).
The study found significant sexual dysfunction and decreased semen parameters in young men with hidradenitis suppurativa, specifically when the gluteal-genital area was involved. Therefore, fertility and sexual function should be evaluated as part of the management of these patients, and when relevant, semen cryopreservation should be discussed. These findings should prompt further research toward implementing a standard of care.
Conclusion:
The association between HS in reproductive-age men and impaired semen parameters and sexual function has considerable clinical relevance. These findings suggest that fertility and sexual function should be routinely assessed as part of the multidisciplinary management of HS in young men, specifically those with gluteal and genital lesions.
Cited Research:
- Association between Hidradenitis Suppurativa and Abnormalities in Semen Parameters and Sexual Function: A Pilot Study: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and does not discriminate. Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
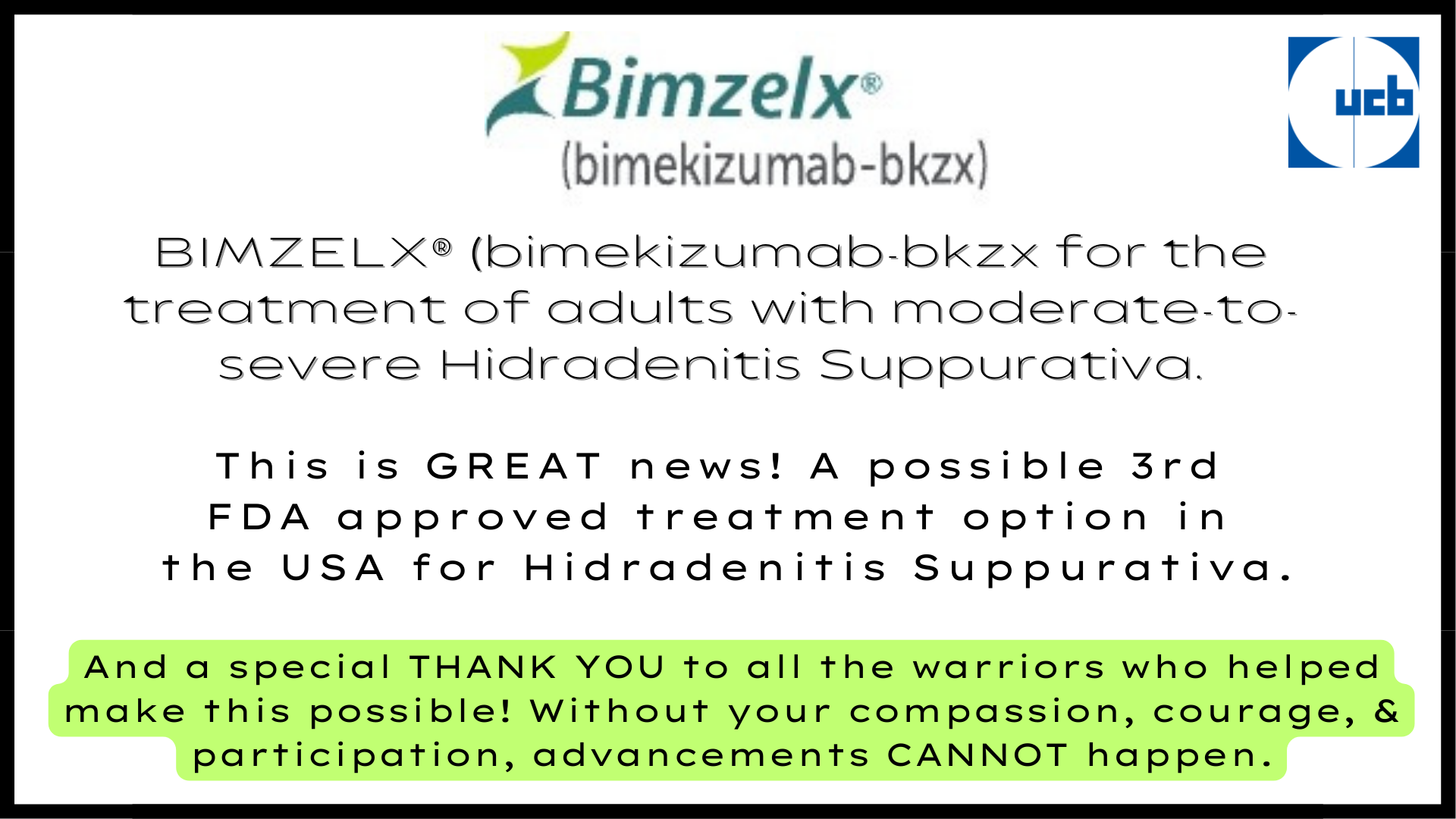
BIMZELX® (bimekizumab) THIRD FDA approved treatment option approved
The THIRD FDA approved treatment for Hidradenitis Suppurativa. As of 11-20-24
The European Commission already GRANTED marketing authorization for BIMZELX in April 2024. That's great to hear!
UCB, a global biopharmaceutical company, announced that the U.S. Food and Drug Administration (FDA) has accepted for review the supplemental Biologics License Application for BIMZELX® (bimekizumab-bkzx) for the treatment of adults with moderate-to-severe hidradenitis suppurativa (HS). This was based on data from phase 3 BE HEARD trials.
"UCB also announced that the European Commission GRANTED marketing authorization for BIMZELX for the treatment of active moderate-to-severe HS in adults with an inadequate response to conventional systemic HS therapy."
“Publication of results from the BE HEARD I and II trials in The Lancet, a world-leading medical journal, reflects the significance of these data to the dermatology community. People living with hidradenitis suppurativa face high unmet medical needs. The positive results from these trials support global regulatory submissions for BIMZELX in this chronic inflammatory skin disease,” said Emmanuel Caeymaex, Executive Vice President, Head of Patient Impact, Chief Commercial Officer, UCB.
This is outstanding for the European community and VERY promising for the United States and globally. Many more options are in the pipeline.
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Information posted on 11-2024
- Patients treated with BIMZELX® (bimekizumab-bkzx) demonstrated clinically meaningful improvements in skin pain up to 48 weeks, across various assessed outcomes
- At Week 16, patients treated with BIMZELX demonstrated greater draining tunnel reductions versus placebo that were sustained or improved to Week 48
- Disease-associated pain and draining tunnels can highly impact the quality of life of people living with moderate-to-severe hidradenitis suppurativa
The European Commission already GRANTED marketing authorization for BIMZELX in April 2024. That's great to hear!
UCB, a global biopharmaceutical company, announced that the U.S. Food and Drug Administration (FDA) has accepted for review the supplemental Biologics License Application for BIMZELX® (bimekizumab-bkzx) for the treatment of adults with moderate-to-severe hidradenitis suppurativa (HS). This was based on data from phase 3 BE HEARD trials.
"UCB also announced that the European Commission GRANTED marketing authorization for BIMZELX for the treatment of active moderate-to-severe HS in adults with an inadequate response to conventional systemic HS therapy."
“Publication of results from the BE HEARD I and II trials in The Lancet, a world-leading medical journal, reflects the significance of these data to the dermatology community. People living with hidradenitis suppurativa face high unmet medical needs. The positive results from these trials support global regulatory submissions for BIMZELX in this chronic inflammatory skin disease,” said Emmanuel Caeymaex, Executive Vice President, Head of Patient Impact, Chief Commercial Officer, UCB.
This is outstanding for the European community and VERY promising for the United States and globally. Many more options are in the pipeline.
Cited Research:
- UCB receives European Commission approval for BIMZELX[®](bimekizumab) as the first IL-17A and IL-17F biologic for moderate to severe hidradenitis suppurativa: See Here
- Anticipated FDA Approval of Bimekizumab for HS: Insights From Investigator Christopher Sayed, MD: See Here
- BIMZELX® 48-Week Phase 3 Analyses in Moderate-to-Severe Hidradenitis Suppurativa Showed Sustained Improvements in Skin Pain and Draining Tunnel Count: See Here
Special Note: Researched, compiled, and written by Denise Fixsen -.Ensuring the utilization of reliable and applicable sources.
Medical Disclaimer: This content is solely for information, education, and support. The purpose is not to serve as a replacement for professional medical advice, diagnosis, or treatments.
Information posted on 11-2024
HS Research
FIND Hidradenitis Suppurativa Research
HERE
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024
HERE
Addressing misconceptions and stigmas that might be found in the cited research / articles: Hidradenitis Suppurativa is a complicated condition that cannot be simplified to only the immune system, hair follicles, follicular occlusion, microbiome disturbance, or biofilm. HS can display diverse clinical presentations in terms of appearance, characteristics, and size. While HS may occasionally manifest as small bumps or acne-like formations, it doesn’t mean this is always the case. In fact, abscesses can grow to the size of a cantaloupe or even bigger. Hidradenitis has the potential to develop in any region where hair follicles are present, despite hair growth. HS can occur in areas without skin folds, or friction. And areas of the body that are prone to skin folds and high friction. HS is not a gland illness and affects individuals of all ages, races, sexual orientations, beliefs, disabilities, blood types, sizes, shapes, and locations without discrimination. *Involving HS patients fully in a global study race and gender is needed before experts can make a concrete decision on prevalence.
Information posted on 09-15-2024